Prediabetes presents a critical stage where blood sugar levels are elevated beyond normal but not yet high enough to be classified as diabetes. This condition signals an increased risk of developing type 2 diabetes, yet it also offers a window of opportunity for intervention through dietary and lifestyle modifications. Emphasizing that prediabetes can often be reversed through lifestyle changes, this article explores the pivotal role of diet in managing prediabetes and provides practical strategies for maintaining healthy blood sugar levels, with the ultimate goal of reversing type 2 diabetes.
The Importance of Diet in Prediabetes Diet Management
The Centers for Disease Control and Prevention (CDC) underscore the efficacy of lifestyle changes in diabetes prevention, clarifying that type 2 diabetes cannot be cured but highlighting that prediabetes is often reversible. Specifically, individuals who achieve a 5–7% weight reduction and incorporate 150 minutes of weekly exercise can lower their risk of developing type 2 diabetes by 58%, with an even greater effect observed in those over 60. A diet conducive to weight management and prediabetes control emphasizes high fiber, low added sugars, and nutrient density, featuring a variety of vegetables, whole grains, lean proteins, legumes, and healthy fats—key components in meals to reverse Type 2 diabetes.
Dietary Components for Prediabetes Diet:
- High-Fiber Foods: Slow-digesting foods, such as whole grains and high-fiber items, gradually release sugars into the bloodstream, aiding in blood sugar control and supporting weight management, heart health, and digestive wellness.
- Carbohydrates: Carbohydrates are crucial for a balanced diet, yet intake should be tailored to individual health needs, activity levels, and lifestyle, with a focus on minimizing added sugars.
- Non-Starchy Vegetables: Opting for low-carbohydrate vegetables over starchy counterparts can enrich the diet with essential nutrients while managing carbohydrate intake.
- Glycemic Index (GI): Understanding the GI of foods can guide selections that prevent rapid blood sugar spikes, with a preference for lower GI options that include fiber-rich fruits and whole grains over refined products.
Understanding the Glycemic Index
The Glycemic Index (GI) categorizes carbohydrate-containing foods by how significantly they raise blood glucose levels. With a scale from 0 to 100, the GI measures the speed at which foods cause our blood sugar to rise. Foods scoring closer to 100 have a rapid effect on blood sugar levels, while those near 0 have a minimal impact.
Overview of Average GI Values
The GI values of foods can vary based on brand and preparation. Here’s a general guide to the average GI values for several common foods and beverages:
- Potatoes: 71
- Rice: 67
- Bread: 64
- Breakfast Cereals: 61
- Pasta: 52
- Fruits: 51
- Cookies: 49
- Confectionery: 48
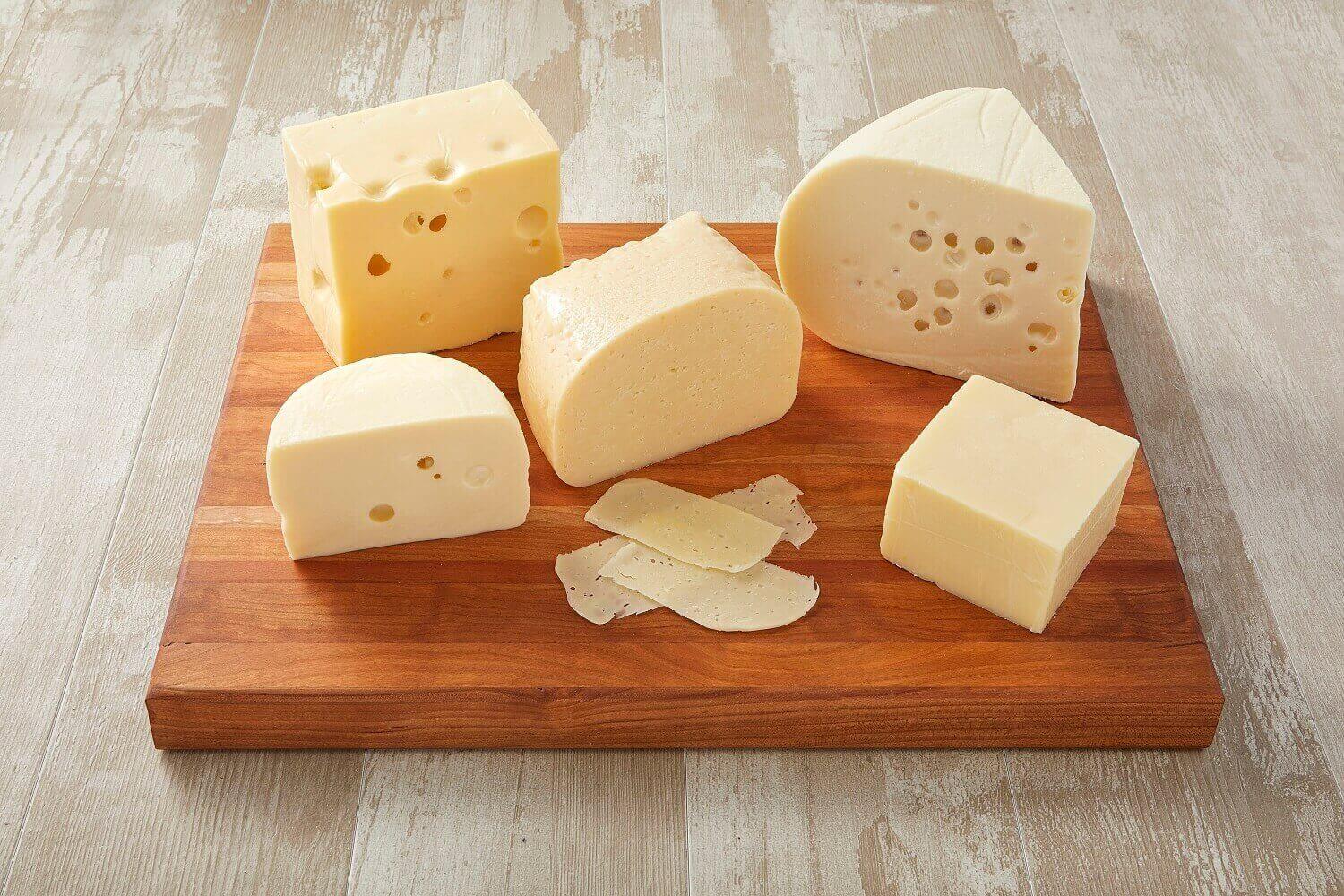
- Dairy Products: 35
- Nuts: 22
Note that individual GI values can differ from one specific item to another, such as the variation in sweetness between different types of apples.
Determinants of GI Scores
High-fiber foods, like fruits and whole grains, generally have lower GI scores compared to those with refined ingredients. This is due to how the body processes refined carbohydrates and sugars, leading to rapid increases in blood sugar, or “sugar spikes.” Therefore, refined and high-sugar foods typically exhibit higher GI scores, exemplified by the difference between white and wholemeal bread’s GI values.
For individuals with prediabetes, it’s advisable to limit high-GI foods to prevent sudden blood sugar elevations. Yet, it’s crucial to recognize that the total carbohydrate intake influences blood sugar levels more significantly than the GI scores of individual foods.
Tips for Choosing Low-GI Foods
To assist those aiming for a low-GI diet, consider the following guidelines:
- Foods with natural sugars, such as fruits, usually have lower GI scores than those with added refined sugars.
- Whole, unprocessed foods are likely to have lower GI values than those made from refined grains (e.g., white bread versus whole grain bread).
- Non-starchy vegetables, sweet potatoes, legumes, and whole fruits typically have lower GI scores compared to white starchy vegetables like potatoes.
- The ripening process can increase the sugar content and GI score of fruits and vegetables.
- Certain types of rice, such as parboiled, basmati, and brown rice, have lower GI values than short-grain or jasmine rice.
- Rolled or steel-cut oats are preferable to quick-cooking oatmeal for those watching their GI intake.
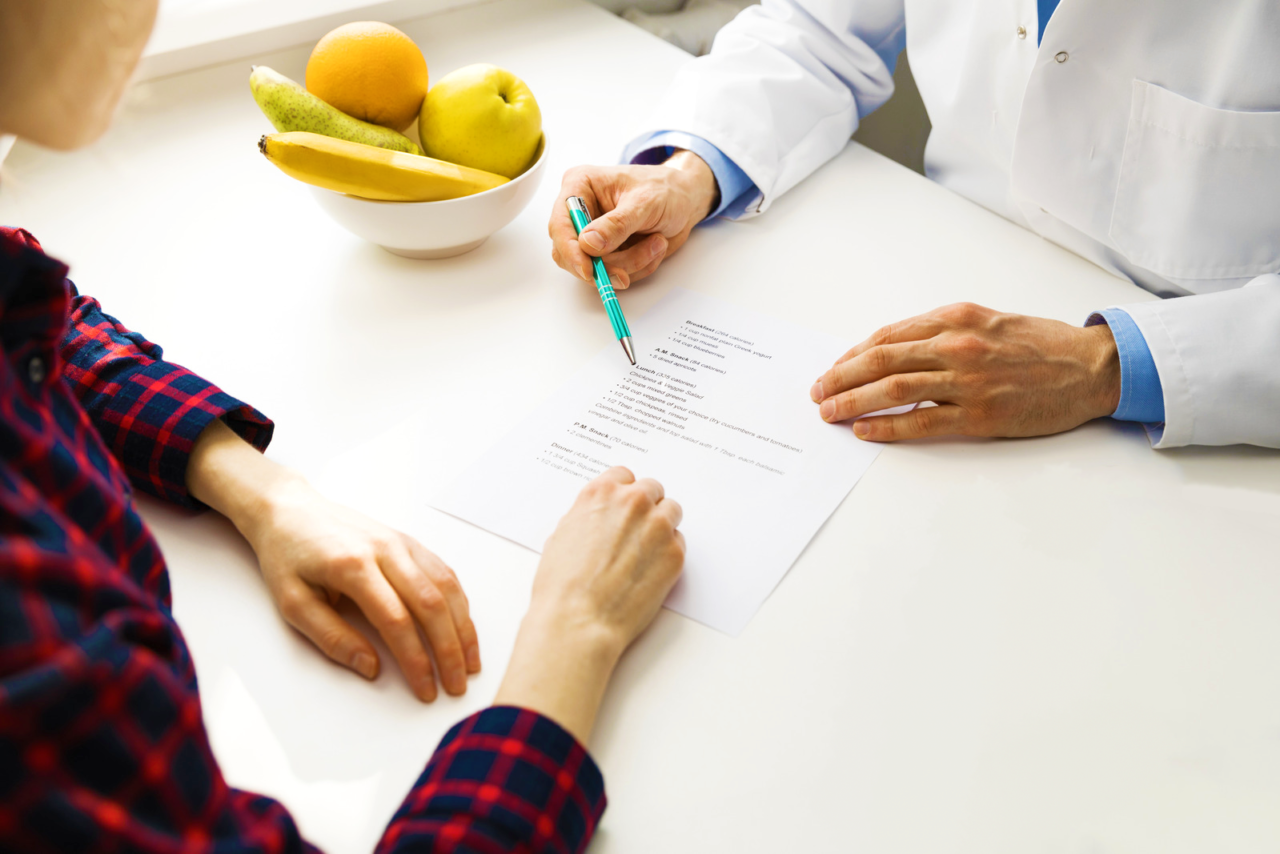
While the benefits of a low-GI diet for prediabetes management are supported by some research, it’s not universally conclusive. Therefore, consulting with a healthcare provider or dietitian for personalized dietary advice is recommended.
Foods to Prioritize and Limit for Prediabetes diet:
- Protein Choices: Incorporating proteins such as tofu, lean meats, and low-fat dairy can balance the diet without excessive carbohydrates or fats.
- Alcohol Consumption: Moderating alcohol intake is advised to manage weight and reduce diabetes risk. Opting for low carb alcoholic drinks, and exercising caution against sugary mixers for those who choose to drink, is recommended.
- Limiting Certain Foods: Attention to overall calorie intake and limiting sugar-sweetened beverages, foods high in added sugars, refined carbohydrates, and saturated fats can mitigate the risk of diabetes and cardiovascular diseases.
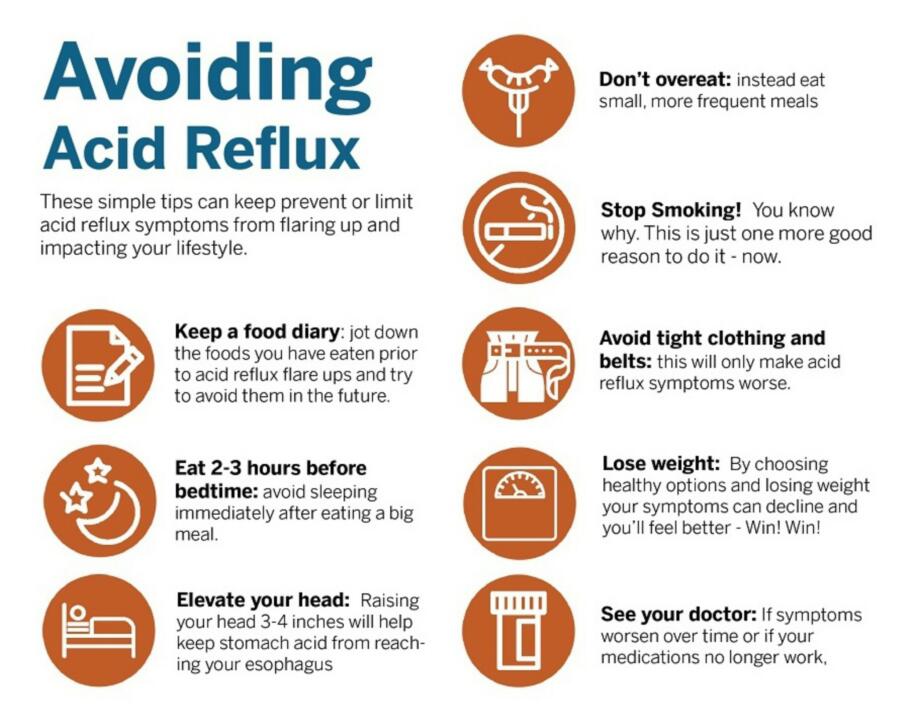
Strategies for Eating Well with Prediabetes Diet:
- Regular, Balanced Meals: Maintaining steady blood sugar levels involves consuming regular, balanced meals that include a mix of proteins, fats, and carbohydrates.
- The Plate Method: This technique aids in portion control, ensuring a healthy balance of non-starchy vegetables, proteins, and carbohydrates.
- DASH Diet: Following the Dietary Approaches to Stop Hypertension (DASH) diet, which emphasizes vegetables, fruits, whole grains, and lean proteins, can support blood sugar management.
Lifestyle Considerations Beyond Prediabetes Diet:
Complementing dietary adjustments with regular physical activity is crucial for weight loss and improved insulin sensitivity. Strategies include engaging in activities like swimming, brisk walking, and strength training, alongside considering medication if recommended by a healthcare provider.
Is Feeling Sleepy After Eating a Sign of Diabetes?
Many wonder, is feeling sleepy after eating a sign of diabetes? While it can be a symptom, particularly if meals are high in carbohydrates or sugar, it’s also common in the general population. Monitoring other symptoms and blood sugar levels is key to understanding your health status.
Customizing Your Approach for the Prediabetes Diet:
There is no one-size-fits-all diet for prediabetes, highlighting the importance of consulting with healthcare professionals for personalized advice. A combination of informed dietary choices, an active lifestyle, and regular monitoring can significantly reduce the progression from prediabetes to diabetes, emphasizing the power of proactive health management. By embracing these comprehensive strategies, individuals with prediabetes can navigate their condition effectively, paving the way for a healthier future.
Meal Planning for Prediabetes Management
For individuals newly diagnosed with prediabetes, making dietary choices can seem daunting. Here are some tips on what to eat and what to avoid to help manage your condition:
Meal Ideas
| Meal | What to Eat | What to Avoid |
|---|---|---|
| Breakfast | – Eggs – Rolled or whole oats – Wholemeal bread – Unsweetened peanut butter – Fruit – Up to 4 ounces of 100% fruit juice with no added sugar – Coffee or tea without sugar | – White bread and bagels – Sweetened breakfast cereals – Sweetened juices – Specialty coffee drinks with added sugar |
| Lunch | – Beans on wholemeal toast – Brown rice, lentils, and salad with a dash of olive oil – Homemade vegetable soup – An apple, pear, melon, or berries | – Bagels, baguettes, and other white or refined bread – Burgers and fast food items – Salad dressings high in added sugars |
| Dinner | – Salmon with yam or sweet potato, leafy greens, and asparagus – Baked chicken with wholemeal pasta and homemade tomato sauce, salad on the side | – Pizza – Premade sauces – Fatty meats |
| Snack | – Nuts – Fruit – Plain, unsweetened yogurt | – Candy – Premade “health” bars with high added sugar |
Guidance for Healthy Eating
Adapting to a prediabetes-friendly diet involves focusing on whole, unprocessed foods and avoiding items high in added sugars and refined carbohydrates. Following a simple pre diabetic meal plan, the meal suggestions aim to balance nutritious food choices throughout the day, from a protein-rich breakfast to a vegetable-packed dinner. Snacking on whole foods like nuts and fruit as part of this straightforward approach can help maintain stable blood sugar levels and prevent overeating during meals. Tailoring your diet with this easy-to-follow plan not only aids in managing prediabetes but also supports overall health and well-being, making it a practical solution for those looking to improve their dietary habits effectively.
References:
- Atkinson, F. S., et al. (2021). “International Tables of Glycemic Index and Glycemic Load Values 2021: A Systematic Review,” Journal of the American College of Nutrition.
- Astrup, A., et al. (2019). “Effects of Full-Fat and Fermented Dairy Products on Cardiometabolic Disease: Food is More Than the Sum of its Parts,” Advances in Nutrition.
- Campbell, A. P. (2017). “DASH Eating Plan: An Eating Pattern for Diabetes Management,” Diabetes Spectrum.
- Drehmer, M., et al. (2015). “Total and Full-Fat, but Not Low-Fat, Dairy Product Intakes are Inversely Associated with Metabolic Syndrome in Adults,” The Journal of Nutrition.
- Dunkley, A. J., et al. (2014). “Diabetes Prevention in the Real World: Effectiveness of Pragmatic Lifestyle Interventions for the Prevention of Type 2 Diabetes and of the Impact of Adherence to Guideline Recommendations: A Systematic Review and Meta-analysis,” The Lancet Diabetes & Endocrinology.
- Farvid, M. S., et al. (2014). “Glycemic Index, Glycemic Load, and Their Association with Glycemic Control Among Patients with Type 2 Diabetes,” The American Journal of Clinical Nutrition.