Having diabetes means nutrition and physical activity play a crucial role in maintaining a healthy lifestyle. Not only do they offer various benefits, but they also help keep your blood glucose levels in check. Balancing what you eat, how much you eat, and when you eat is essential for managing blood glucose, along with any diabetes medicine you may take.
It’s understandable that making changes to your diet and becoming more active can seem daunting. However, starting with small adjustments and seeking support from your family, friends, and healthcare team can make the process of creating and following a diabetes diet easier.
The good news is that having diabetes doesn’t mean giving up your favorite foods entirely. You may need to enjoy them in moderation or adjust portion sizes. Your healthcare team will work with you to create a personalized diabetes meal plan that suits your needs and preferences.
When it comes to eating with diabetes, the key is to have a diverse range of healthy foods from all food groups, as outlined in your meal plan:
- Vegetables – Nonstarchy options like broccoli, carrots, greens, peppers, and tomatoes, as well as starchy ones like potatoes, corn, and green peas.
- Fruits – Include oranges, melons, berries, apples, bananas, grapes, and other fruits you enjoy.
- Grains – Aim for at least half of your grains to be whole grains, like wheat, rice, oats, cornmeal, barley, and quinoa. This includes foods like bread, pasta, cereal, and tortillas.
- Protein – Opt for lean meats, chicken or turkey without the skin, fish, eggs, nuts, peanuts, dried beans, certain peas like chickpeas and split peas, and meat substitutes like tofu.
- Dairy – Choose nonfat or low-fat options such as milk, yogurt, and cheese. If you have lactose intolerance, consider lactose-free milk.
- Heart healthy fats – Include heart-healthy fats in your diet, such as oils that are liquid at room temperature (canola and olive oil), nuts, seeds, heart-healthy fish like salmon, tuna, and mackerel, and avocados. Use oils for cooking instead of butter, cream, shortening, lard, or stick margarine.
With the right approach to food and physical activity, you can better manage your blood glucose levels, blood pressure, and cholesterol, achieve or maintain a healthy weight, prevent or delay diabetes-related problems, and overall, feel good and have more energy.
Which foods and drinks should I cut back on if I have diabetes?
Limit the following:
- Fried foods and foods high in saturated and trans fats.
- High-salt foods (sodium).
- Sweets like baked goods, candy, and ice cream.
- Beverages with added sugars, such as juice, regular soda, and energy drinks.
Instead of sweetened drinks, opt for water. If you enjoy coffee or tea, consider using a sugar substitute. If you drink alcohol, do so in moderation – no more than one drink a day if you’re a woman, or two drinks a day if you’re a man. Be cautious, especially if you use insulin or diabetes medications that increase insulin production, as alcohol can cause your blood glucose levels to drop too low. It’s a good idea to have some food when drinking alcohol.
Timing your meals: When to eat with diabetes
When it comes to meal timing, some people with diabetes benefit from eating at consistent times each day, while others can be more flexible. Depending on your diabetes medications or insulin type, you may need to consume the same amount of carbohydrates at the same time daily. For those on “mealtime” insulin, eating schedules can be more flexible.
Skipping or delaying meals when using certain diabetes medications or insulin can lead to dangerously low blood glucose levels. Consult your healthcare team to determine the best eating schedule for you, especially before and after physical activity.
Managing diabetes: how to find the right portion sizes
Maintaining the right portion sizes is crucial for managing blood glucose levels and weight. Your healthcare team can help you determine how much food and how many calories you should consume daily. To lose weight, focus on consuming fewer calories and replacing unhealthy foods with lower-calorie, low-fat, and low-sugar options.
If you have diabetes, are overweight or obese, and plan to become pregnant, it’s advisable to lose any excess weight before conceiving. For more information on planning for pregnancy with diabetes, consult your healthcare provider.
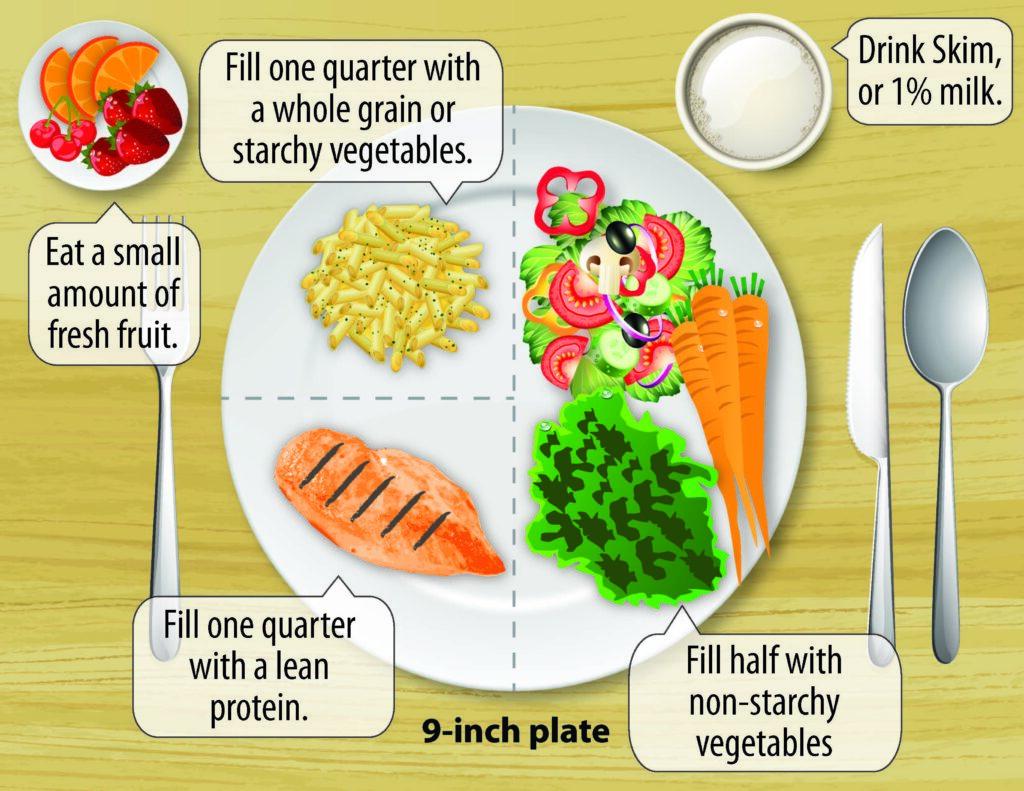
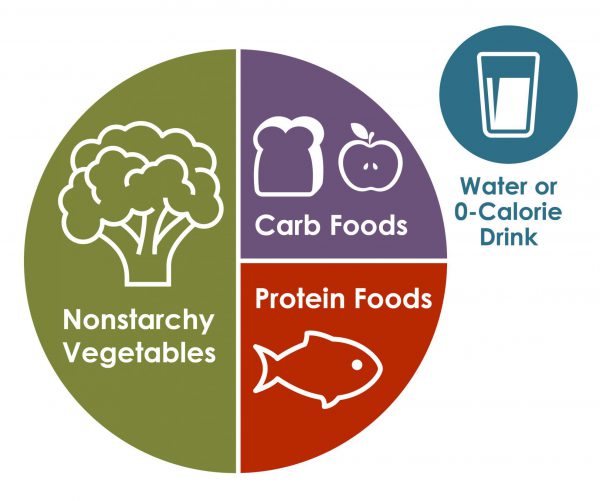
To help plan your meals, two common approaches are the plate method and carbohydrate counting. Talk to your healthcare team to decide which method suits you best. The plate method simplifies portion control and doesn’t require counting calories. Use a 9-inch plate and fill half of it with non-starchy vegetables, one-fourth with a protein source, and the last one-fourth with a grain or starch. You can include starchy vegetables like corn and peas. Additionally, have a small bowl of fruit or a piece of fruit, along with a small glass of milk as part of your meal plan.
Easily managing portions and carbs for diabetes
Controlling portion sizes and counting carbs can be simpler than you think! You don’t need any fancy gadgets – everyday objects and your hand can help. For meat or poultry, one serving is about the size of your palm or a deck of cards. A 3-ounce serving of fish is like a checkbook, and one serving of cheese is approximately six dice.
To estimate portions of carbs, here are some helpful comparisons:
- 1/2 cup of cooked rice or pasta is about the size of a rounded handful or a tennis ball.
- A pancake or waffle should be around the size of a DVD.
- Two tablespoons of peanut butter equals a ping-pong ball.
Carb counting is another useful tool, especially for those on insulin. It involves tracking the amount of carbohydrates you consume daily since they have a significant impact on your blood glucose levels. You’ll find carbohydrates in foods like starches, fruits, milk, and sweets. When counting carbs:
- Learn which foods contain carbohydrates.
- Read the Nutrition Facts label, or get the hang of estimating carbs in your meals.
- Add up the grams of carbs from each food to get your total for each meal and the day.
While carb counting is crucial for people on insulin, not everyone with diabetes needs to do it.
Remember to focus on healthier carb choices, like fruits, vegetables, whole grains, beans, and low-fat or nonfat milk. Limit carbs with added sugars and refined grains (e.g., white bread, white rice) for better blood glucose management.
Your healthcare team can help you create a personalized eating plan that suits your needs best.
References:
- Chandalia M, Garg A, Lutjohann D, von Bergmann K, Grundy SM, Brinkley LJ (May 2000). “Beneficial effects of high dietary fiber intake in patients with type 2 diabetes mellitus”. The New England Journal of Medicine.
- Bashier A, Bin Hussain A, Abdelgadir E, Alawadi F, Sabbour H, Chilton R (2019). “Consensus recommendations for management of patients with type 2 diabetes mellitus and cardiovascular diseases”. Diabetology & Metabolic Syndrome.
- Scott SN, Anderson L, Morton JP, Wagenmakers AJ, Riddell MC (May 2019). “Carbohydrate Restriction in Type 1 Diabetes: A Realistic Therapy for Improved Glycaemic Control and Athletic Performance?”. Nutrients.
- American Diabetes Association Professional Practice Committee (January 2019). “Standards of Medical Care in Diabetes-2019”. Diabetes Care.
- Melina, Vesanto; Craig, Winston; Levin, Susan (December 2016). “Position of the Academy of Nutrition and Dietetics: Vegetarian Diets”. Journal of the Academy of Nutrition and Dietetics.





























