In the dynamic world of medical technology, one of the most significant advancements reshaping diabetes management is the use of CGMs in diabetes care. CGMs stand for Continuous Glucose Monitors, and these devices are gaining increasing acceptance for their detailed and round-the-clock tracking capabilities, offer a new lens through which individuals can view and manage their diabetes.
Understanding CGMs in Diabetes Care
At its core, a CGM is an advanced tool designed to offer a comprehensive and ongoing analysis of glucose levels. Traditional methods like finger stick tests require a manual check, where a drop of blood is placed on a test strip to provide a snapshot of the glucose level at a specific moment. While effective, this method offers a limited view, akin to seeing a single frame of a movie rather than the entire film.
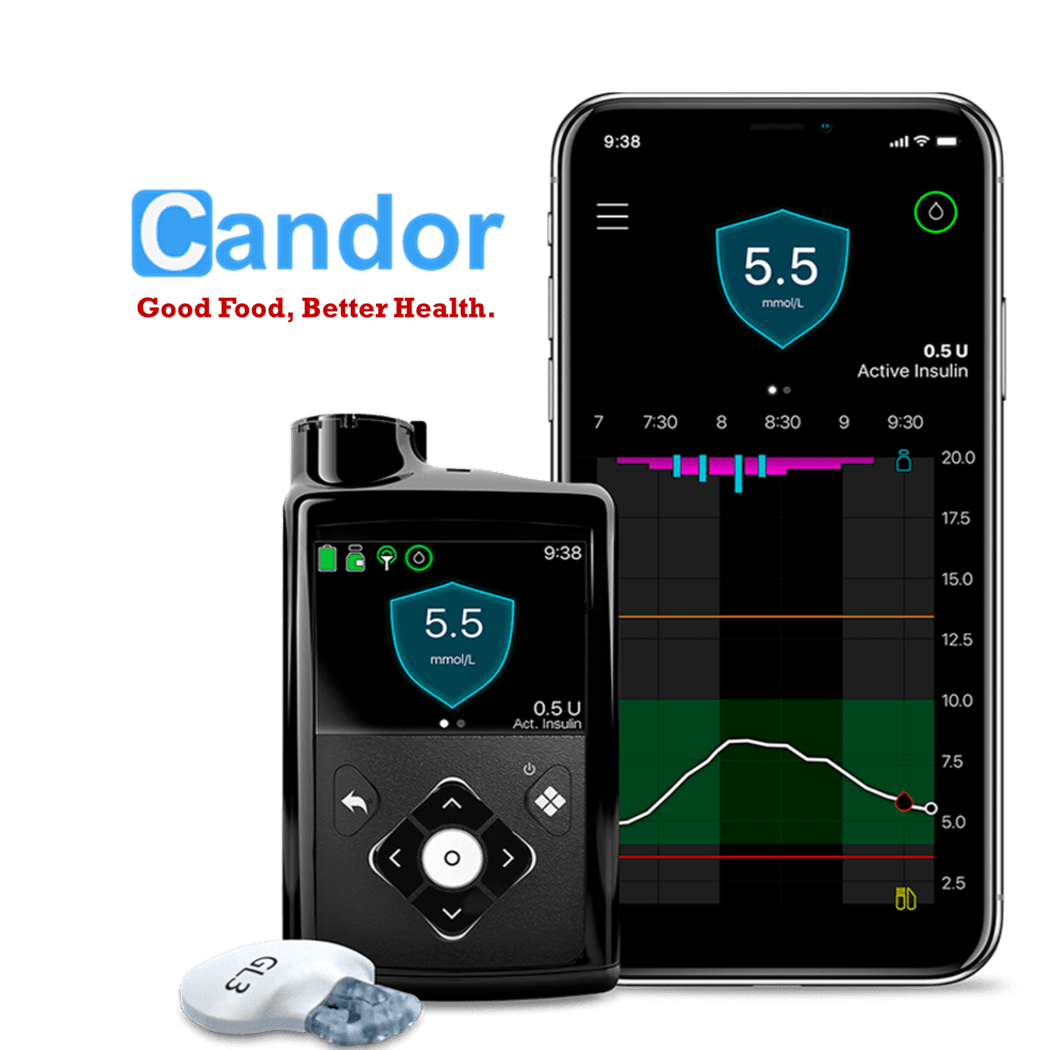
CGMs, on the other hand, provide a continuous stream of data, capturing the nuances of glucose fluctuations over time. This is done through a small sensor with a thin needle that is gently inserted under the skin. This sensor is attached to a transmitter which relays information to a receiving device such as a smartphone app, smartwatch, or a specialized monitor.
The Working Mechanism of CGMs
The science behind CGMs involves measuring glucose levels in the interstitial fluid – the fluid surrounding the body’s cells. The sensor’s electrode performs frequent readings, offering a detailed graph of glucose trends. This real-time data transmission allows users to observe how various activities and choices, like eating certain foods or physical exercise, impact their glucose levels.
Continuous Glucose Monitors (CGMs), regardless of the brand, essentially function in the same way, comprising three key components:
- Monitor/App: This component, which could be a dedicated monitor or an app on your smart device, displays your current blood sugar levels, historical data, and trends. These trends are useful for predicting future rises and falls in your blood sugar levels.
- Sensor: This is a tiny cannula wire positioned under the skin, constantly measuring your blood sugar levels.
- Transmitter: Attached to the sensor, the transmitter relays blood sugar information to your device, be it a monitor or a smartphone. Note that intermittent monitors do not include this part, a distinction I’ll explain later.
CGMs offer a significant advantage over traditional fingerstick monitoring by providing continuous, automatic readings. This continuous tracking allows for the observation of trends in blood sugar levels, including both highs and lows. Notably, many CGMs come with customizable alarms to notify the patient or their caregiver of any dramatic changes in blood sugar levels.
Intermittent vs. Real-Time CGMs:
The primary distinction between CGM devices lies in their monitoring type: intermittent versus real-time.
- Intermittent Monitors: These require the user to manually scan the sensor using a reader or smartphone to view glucose levels. They do not feature alarms, and users must check their levels manually.
- Real-Time Monitors: These devices continuously track glucose levels and provide alerts for significant changes. They feature alarms to notify users of any issues with their glucose levels.
Advantages of Using a CGM
One of the primary benefits of CGMs is the depth of insight they provide. Users can detect patterns and trends in their glucose levels, making it easier to understand the impact of lifestyle choices and medications. Additionally, CGMs offer critical real-time alerts. These alerts are particularly useful for individuals experiencing significant glucose variability, as they can signal the need for immediate action, such as in cases of nocturnal hypoglycemia.
Some CGMs are also integrated with insulin pumps, further streamlining diabetes management by automatically adjusting insulin doses based on real-time glucose readings. This integration represents a significant step towards more personalized and precise diabetes care.
Challenges and Considerations in CGM Use
Despite their advantages, CGMs are not without limitations. One challenge is their lag time in detecting rapid glucose changes, which can be around 10 minutes behind finger stick readings. They also tend to read lower than finger stick tests, necessitating a manual check for verification in certain scenarios.
Physical discomfort from the sensor and alarm fatigue are other concerns. The constant stream of data and alerts can sometimes be overwhelming, leading to a phenomenon where users may become desensitized to the information provided.
Another important consideration is the cost. CGMs, often not fully covered by insurance, can represent a significant out-of-pocket expense. This factor can limit accessibility for many individuals who could benefit from this technology.
In Summary
CGMs represent a transformative tool in diabetes management, offering detailed insights into glucose patterns and enabling more informed decision-making. While they are a significant step forward in diabetes care, it’s essential to weigh their benefits against the challenges and costs involved. For those considering a CGM, it’s crucial to have a comprehensive discussion with healthcare providers to understand how this technology can be best utilized in the context of their individual health needs and circumstances.
References:
- “Continuous glucose monitoring systems – Current status and future perspectives of the flagship technologies in biosensor research,” Biosensors, 2021.
- “The Evidence Base for Continuous Glucose Monitoring,” Anne L. Peters, MD, ADA Clinical Compendia, 2018.