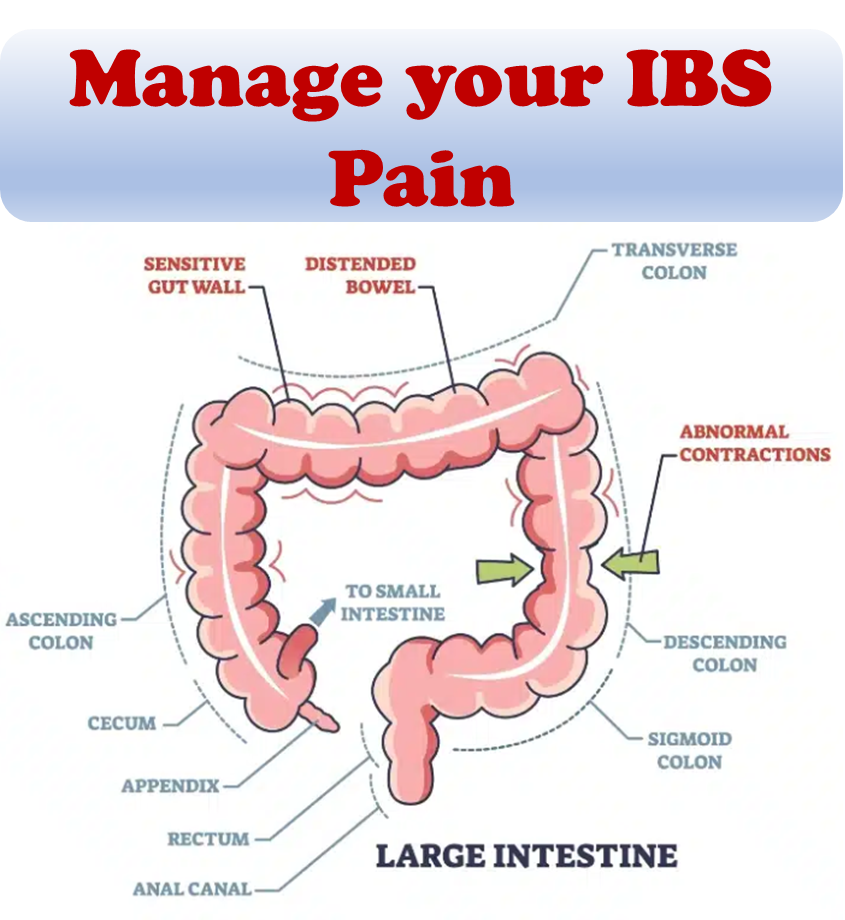
Irritable bowel syndrome (IBS) doesn’t come with a manual. We cover a list of 10 coping strategies for your IBS here since these coping strategies may not be immediately apparent for managing this invisible, chronic condition with embarrassing physical symptoms.
To navigate IBS effectively, it’s crucial to understand common pitfalls and learn how to sidestep them.
Challenge the Notion of Helplessness
Despite the discouraging notion that “there is nothing that can be done” for IBS, many individuals find relief through multiple strategies. Exploring various approaches, such as dietary modifications, stress management techniques, and medical interventions, can contribute to easing symptoms. Reading IBS success stories and memoirs often reveals a combination of strategies that individuals have found effective in their unique journeys.
Ditch Unnecessary Diet Restrictions
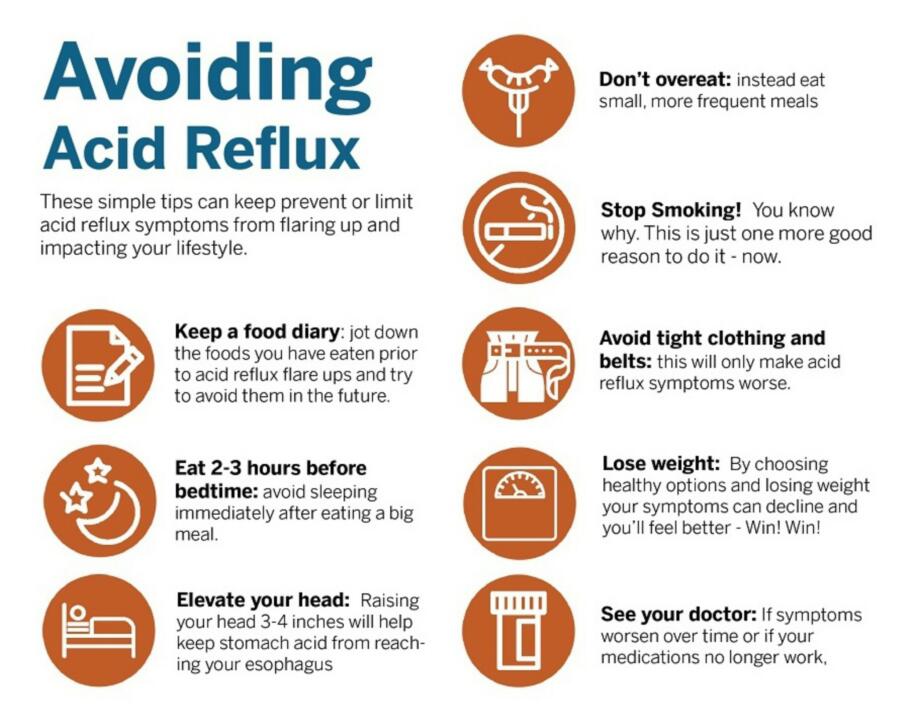
When grappling with IBS symptoms, the instinct to blame the last meal is natural. However, it’s essential to recognize that various factors, such as stress, hormonal changes, or even a large meal, can trigger IBS symptoms. Overly restrictive diets, intended to include only perceived “safe” foods, carry the risk of nutritional deficiencies.
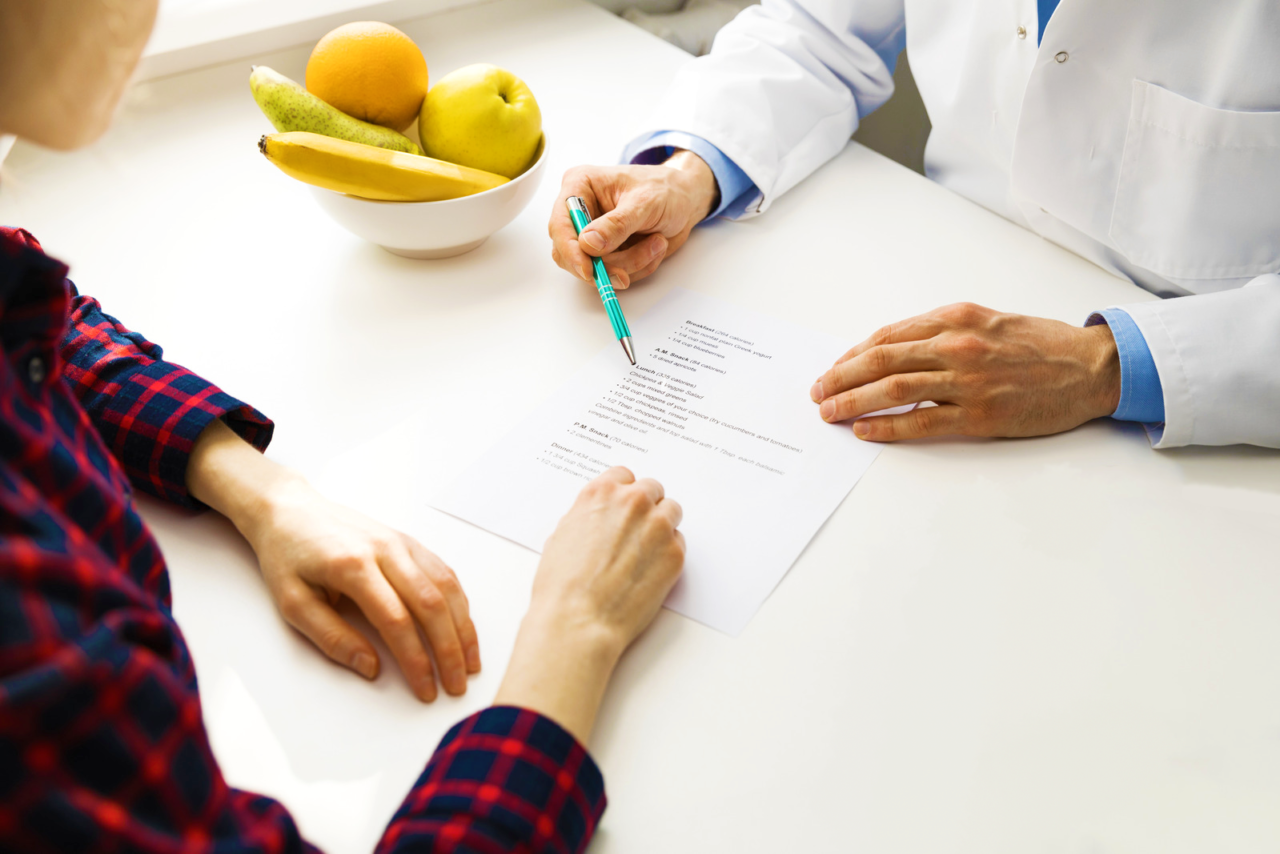
Some individuals with IBS may identify specific food sensitivities through methods like keeping a food diary and following an elimination diet. However, excessive restriction can also arise with the low-FODMAP diet, which, when followed without professional guidance, may lead to missing out on beneficial nutrients from foods with higher FODMAP levels.
Embrace Fiber
Despite common reservations, incorporating fiber into your diet is crucial for maintaining overall digestive health. Gradual integration, starting with whole grains, fruits, and vegetables, can help manage both constipation and diarrhea. It’s worth noting that while bran may be irritating to the digestive system, bulk laxatives, which are essentially fiber supplements, offer a less abrasive alternative.
Choose Empathetic Healthcare Providers
The relationship between healthcare providers and individuals with IBS is integral to effective management. Opting for healthcare professionals who approach IBS with patience and empathy is crucial. If your current provider exhibits signs such as attributing symptoms solely to psychological factors or making you feel unsupported in seeking pain relief, consider exploring alternative healthcare options.
Avoid Junk Food
While the link between IBS and food remains intricate, a considerable number of individuals experiencing relief from their IBS symptoms attribute it to eliminating junk food from their diet. In the short term, this adjustment may pose challenges, as junk food is often readily available and tempting. However, in the long run, steering clear of these nutritionally deficient options can be a pivotal aspect of managing IBS.
Why is junk food detrimental to IBS? Here’s a closer look at some of the reasons:
- High-fat content: Fats in foods can heighten the intensity of intestinal contractions, potentially contributing to abdominal pain.
- Low fiber content: Junk food, lacking true plant material, is often low in fiber. While the relationship between fiber and IBS might be complex, it plays a crucial role in maintaining stool consistency—essential for those with IBS-C or IBS-D.
- Artificial sweeteners: Some artificial sweeteners, especially those ending in “-ol,” have been linked to increased symptoms of gas and bloating.
- Food additives: The health effects of food additives may be a topic of debate, but these ingredients are often added to processed foods for shelf-life extension and aesthetic appeal, not for their nutritional value.
Challenging the notion of helplessness is paramount. Despite common advice suggesting little can be done for IBS, exploring diverse strategies—ranging from dietary adjustments to stress management—can significantly alleviate symptoms. A proactive and comprehensive approach, backed by individualized strategies, emerges as a key theme in effectively managing life with IBS.
Cease Stool Monitoring
The diagnostic process for IBS involves ruling out other diseases, leading to understandable uncertainty. However, compulsive monitoring of stool color and appearance can escalate anxiety and contribute to unnecessary worry. It’s essential to trust in the diagnostic process and refrain from unnecessary vigilance, except in cases where there are specific concerning symptoms, such as the presence of blood in the stool.
Shed Embarrassment
Digestive symptoms are a universal aspect of the human experience, and everyone deals with them in one way or another. Bowel noises and smells are natural occurrences, and while it’s understandable to feel self-conscious, it’s important to recognize that these aspects are a normal part of daily life. Embracing this perspective can alleviate unnecessary stress associated with IBS-related embarrassment.
Stop Keeping IBS a Secret
The decision to keep IBS a secret can inadvertently intensify stress and hinder potential support systems. Opening up to trusted individuals about your condition can foster understanding and pave the way for assistance in meeting your unique needs. Sharing your experience also contributes to breaking down the stigma surrounding digestive health issues.
Release the Quest for Perfection
Living with IBS can bring about a sense of pressure to compensate for missed commitments or activities. However, it’s crucial to recognize that IBS is a health problem, not a personal failing. Overcompensating by taking on extra responsibilities or feeling an obligation to always say yes to requests can exacerbate anxiety, leading to increased symptoms. Setting realistic limits, delegating tasks, and prioritizing self-care are essential strategies for managing IBS-related challenges.
Avoid Social Isolation
While the unpredictable nature of IBS may pose challenges in planning activities, succumbing to social isolation can contribute to a depressed mood state. Seeking out opportunities and activities that uplift your mood and energy levels is crucial. Communicating health-related limitations to others and canceling plans when necessary can help strike a balance between social engagement and self-care.
References:
- Cozma-petruţ A, Loghin F, Miere D, Dumitraşcu DL. (2017) “Diet in irritable bowel syndrome: What to recommend, not what to forbid to patients!” World Journal of Gastroenterology.
- National Institute for Diabetes and Digestive and Kidney Diseases. “Eating, diet, & nutrition for irritable bowel syndrome.”