Indian diet plan for acidity finds its roots in dietary choices. In the diverse tapestry of the Indian diet, characterized by rich flavors and a plethora of spices, understanding how to manage acidity becomes crucial for maintaining digestive health.
The gastrointestinal tract, also known as the digestive tract or alimentary canal, is a long, continuous tube that extends from the mouth to the anus. It plays a crucial role in the digestion, absorption, and elimination of food and waste products from the body. The major organs and structures that make up the gastrointestinal tract include:
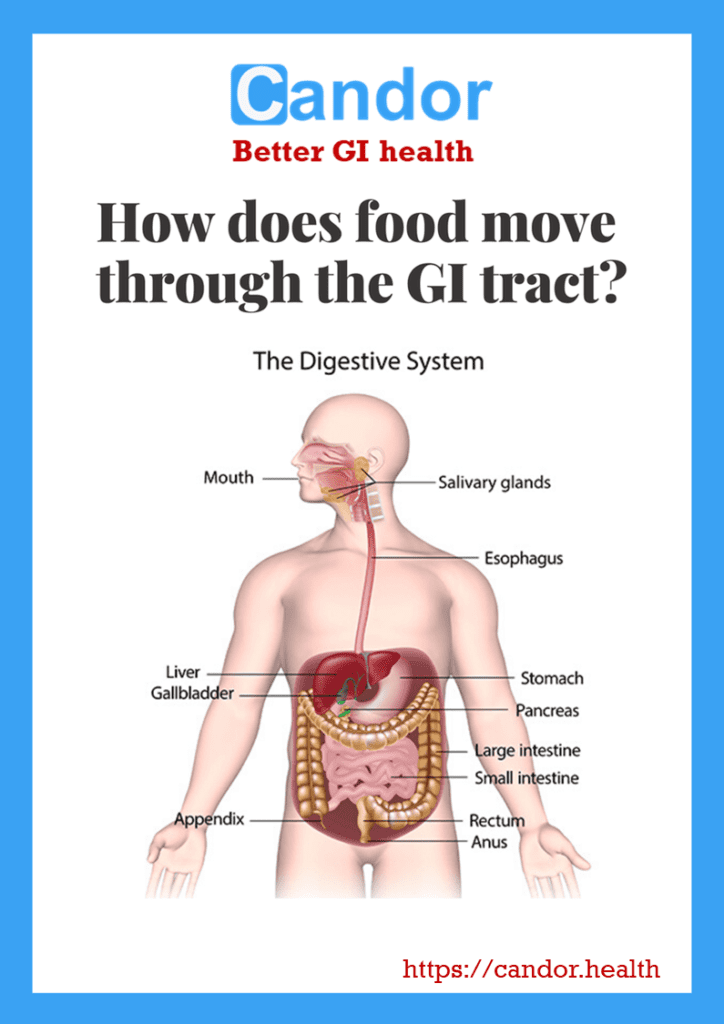
(from How food moves through the digestive system)
- Mouth: The digestive process begins in the mouth, where food is chewed and mixed with saliva, which contains enzymes that help break down carbohydrates.
- Esophagus: This muscular tube connects the mouth to the stomach and transports swallowed food from the mouth to the stomach through a series of coordinated muscle contractions called peristalsis.
- Stomach: The stomach is a muscular organ that receives food from the esophagus. It secretes gastric juices, including acid and enzymes, that further break down food and initiate the digestion of proteins. The stomach also helps regulate the release of food into the small intestine.
- Small Intestine: The small intestine is the longest part of the gastrointestinal tract and is divided into three sections: the duodenum, jejunum, and ileum. It is the primary site for the digestion and absorption of nutrients. Enzymes from the pancreas and bile from the liver help break down fats, proteins, and carbohydrates into their basic building blocks, which are then absorbed through the lining of the small intestine into the bloodstream.
- Liver: While not a part of the digestive tract itself, the liver plays a vital role in digestion. It produces bile, a substance that helps emulsify fats and aids in their digestion and absorption. Bile is stored in the gallbladder and released into the small intestine when needed.
- Pancreas: The pancreas is another accessory organ that assists in digestion. It produces digestive enzymes that are released into the small intestine to further break down carbohydrates, proteins, and fats.
- Large intestine (Colon): The large intestine receives undigested food particles, water, and electrolytes from the small intestine. Its primary function is to absorb water and electrolytes, form and store feces, and facilitate the elimination of waste products from the body.
- Rectum and anus: The rectum is the lower part of the large intestine that stores feces until they are expelled from the body through the anus during defecation.
What is GER?
Gastroesophageal reflux (GER) happens when your stomach contents come back up into your esophagus. Many people have GER once in a while, and GER often happens without causing symptoms. In some cases, GER may cause heartburn, also called acid indigestion. Doctors also refer to GER as: acid indigestion, acid reflux, acid regurgitation, heartburn or reflux.
What is GERD?
Gastroesophageal reflux disease (GERD) is a more severe and long-lasting condition in which GER causes repeated symptoms that are bothersome or lead to complications over time. If you think you may have GERD, you should see your doctor. Researchers estimate that about 20 percent of people in the United States have GERD.
Who is more likely to have GERD?
Anyone can develop GERD. You are more likely to have GERD if you:
– are overweight or have obesity
– are a pregnant woman
– take certain medicines
– smoke or are regularly exposed to secondhand smoke
What causes acidity and reflux issues?
The stomach has glands that release gastric juice, a mix of Hydrochloric acid (HCl), Lipase, and Pepsin, necessary for digestion. Excessive production of this gastric juice leads to a burning sensation in the stomach and beneath the breastbone—commonly known as Acidity. If this persists for over a week, it becomes Gastroesophageal Reflux Disease (GERD).
People often endure this pain quietly or opt for a quick antacid fix, offering temporary relief before the pain returns. Those dealing with Acidity or GERD face challenges in eating, sleeping, and focusing on daily tasks. In GERD, instead of food continuing to the small intestine after interacting with digestive juices, it regurgitates back to the esophagus. This happens due to the malfunctioning of the esophageal sphincter—a circular band of tissue at the base of the esophagus.
Ideally, the sphincter should stay closed once food passes through it. However, in GERD, it relaxes at the wrong times, allowing partially digested food to move back into the esophagus. This regurgitated food is often acidic, causing heartburn—a burning sensation from the stomach to the middle-upper chest. Understanding these digestive disruptions is crucial in dealing with gastric issues and GERD.
GERD or Acidity stems from two primary causes – the improper functioning of the Esophageal Sphincter and the consumption of Acidic Foods.
Causes for the malfunctioning Esophageal Sphincter:
- Obesity: Excess weight, particularly around the abdominal area, adds pressure on the sphincter muscles. This increased pressure makes it challenging for the muscles to keep the sphincter closed after swallowing food.
- Slow Digestion: Normal digestion involves the stomach emptying partially digested food into the small intestines for further processing. Delayed gastric emptying, a slowdown in this process, occurs when food and liquids linger in the stomach for an extended period and move upward into the esophagus. Factors contributing to slow digestion include high-fat content in food, conditions like Diabetes, or the use of specific drugs such as antihistamines, antidepressants, and anti-diarrhea medications.
- Hiatal Hernia: Hiatal Hernia involves a part of the stomach protruding through the diaphragm, the muscle separating the chest cavity and abdomen. This displacement occurs at the junction where the esophagus joins the stomach. The protruding stomach tissue exerts pressure on the esophageal sphincter, leading to the development or worsening of GERD. Hiatal Hernia typically results from weakened tissues or excessive pressure due to physical exertion.
Understanding these distinct factors contributing to GERD or Acidity sheds light on the varied triggers that can disrupt the normal functioning of the digestive system.
Reasons for Stomach Acidity:
- Insufficient Saliva: Saliva plays a crucial role in neutralizing stomach acid. Some medications and issues with salivary gland function can disrupt saliva production, contributing to acidic stomach content.
- GERD Triggers: Smoking, alcohol consumption, cola beverages, orange juice, tomato juice, spicy foods, fatty foods, high-sugar foods, and fried foods are culprits in causing GERD symptoms. These substances impact the nerves of the esophageal sphincter muscle, prompting it to open and reverse the flow of food into the esophagus.
- Dyspepsia or Indigestion: Dyspepsia, also known as functional dyspepsia, refers to recurring abdominal discomfort encompassing pain, gas, bloating, heartburn, nausea, vomiting, belching, and a sour taste in the mouth. The term “functional” implies that there’s no structural issue with the upper digestive area, yet symptoms persist.Causes for Dyspepsia:
- Diet: Certain hard-to-digest foods often exacerbate indigestion.
- Unhealthy Lifestyle.
- Medications like non-steroidal anti-inflammatory drugs (NSAIDs).
- Anxiety or Depression.
- Infection by the bacterium H. Pylori.
- Altered or delayed emptying of food from the stomach into the small intestine, causing bloating and gas.
Understanding the pragmatic causes behind stomach acidity sheds light on the various factors that can disrupt digestive equilibrium. Here are some general tips to manage the issue:
- Meal Timing: Conclude your meals at least 3 hours before bedtime. Avoid immediate sleep after eating, especially if dealing with GERD/Acidity/Heartburn. Keep your head elevated while sleeping.
- Physical Activity: Incorporate regular physical activity, aiming for an hour each day.
- Weight Management: Maintain a healthy weight and, if overweight, embark on a gradual and healthy weight reduction journey.
- Meal Planning: Plan your meals in advance to navigate your diet seamlessly.
- Sleep: Prioritize 8 hours of quality sleep for optimal digestion.
- Stress Management: Integrate meditation and yoga into your routine to effectively manage stress.
- Dining Out: Minimize frequent dining out and make healthy choices when doing so.
- Clothing: Avoid tight-fitting clothes around the abdominal area to prevent constriction.
- Medication Adherence: Take prescribed medications and supplements promptly, consulting both your doctor and nutritionist. Never halt any medication without informing your healthcare professionals.
- Positivity: Cultivate a positive mindset towards your body, recognizing the journey towards well-being.
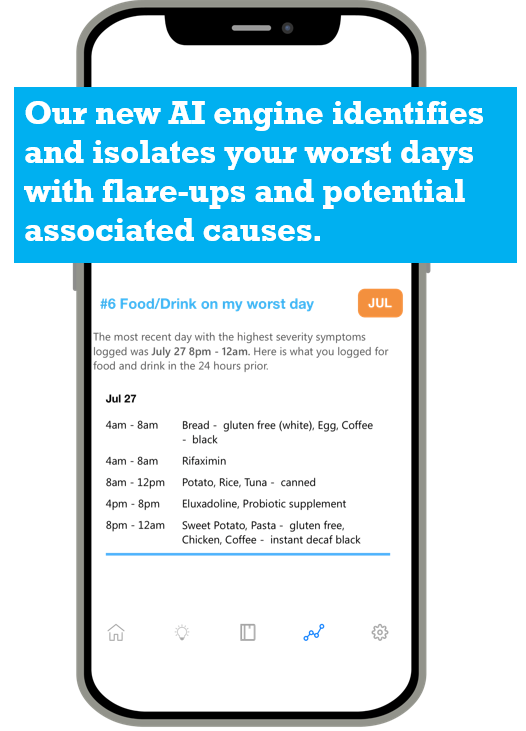
Comprehensive diet tracking and plan
The comprehensive dietary plan is designed not just for immediate relief from symptoms but to establish a lasting shift in your lifestyle, safeguarding against future digestion issues. Even if you happen to deviate from the plan and encounter a recurrence of symptoms, tracking the diet allows you to be flexible with your strategy so you can recalibrate your habits and dietary choices, ensuring ongoing trouble-free digestion.
Week 1
During the initial week, gather essential details about your diet and body. This data will assist you in identifying the most effective ways to alleviate your symptoms. This week is dedicated to raising awareness about your dietary choices and understanding your body’s responses to different foods.
The primary objective for the week is to maintain a detailed record of all your dietary intake. The Candor app allows you to easily log diet and medications and can also identify triggers after a reasonable amount of data has been provided. Examine the timing of the day when symptoms are most pronounced. The culprit behind those symptoms is typically the food consumed in the preceding meal.
Week 2:
Continue the process of collecting and documenting information on your food intake and the associated symptoms. This week, pay attention to your eating habits by recording the time it takes to complete your meals, the pace at which you eat, the quantity consumed, and any snacking habits. In addition to these observations, consider making adjustments to your eating behavior:
- Portion Control: Overeating is a significant contributor to digestive issues. Opt for smaller meals and portion sizes to promote smoother digestive function. Reduce your standard food portions, utilize smaller plates and bowls, resist going for seconds, and avoid overeating when you’re no longer hungry.
- Social Eating: Share mealtime with family members or create a pleasant atmosphere if you’re dining alone. Engage in conversation and make the mealtime enjoyable. Avoid multitasking, such as reading a book or watching television, while eating.
- Consistent Meal Timing: Stick to regular meal timings, consuming meals at the same time each day. Aim to finish dinner early, as GERD and Dyspepsia symptoms tend to worsen during nighttime.
- Eat Slowly and Mindfully: Rapid consumption is another factor linked to digestive problems. Extend your mealtime to 20-30 minutes, making it a relaxed experience rather than a rushed affair. For instance, avoid devouring breakfast hastily in transit; instead, set aside time to sit peacefully and savor your meal. Chew each bite thoroughly before swallowing.
- Hydration Choices: Instead of keeping sugary or alcoholic beverages at hand during meals, opt for a glass of water. Sip water whenever the need for a drink arises.
Week 3 and 4:
Embark on a pivotal phase this week, potentially reshaping your dietary routine as you bid farewell to foods causing issues. Revisit the log you crafted in the initial week and eradicate problematic foods from your diet. If medications or supplements seem to be contributing to your symptoms, engage in a discussion with your physician to explore potential alterations. It’s crucial not to cease any medication without seeking professional advice.
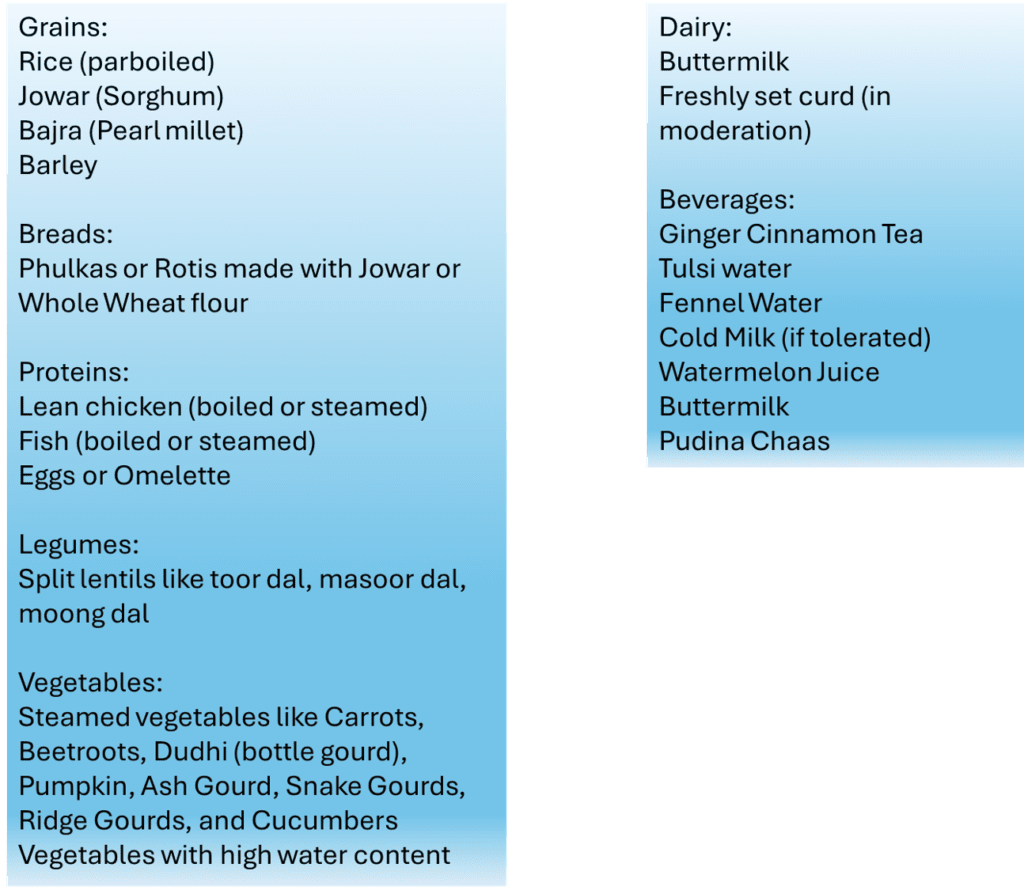
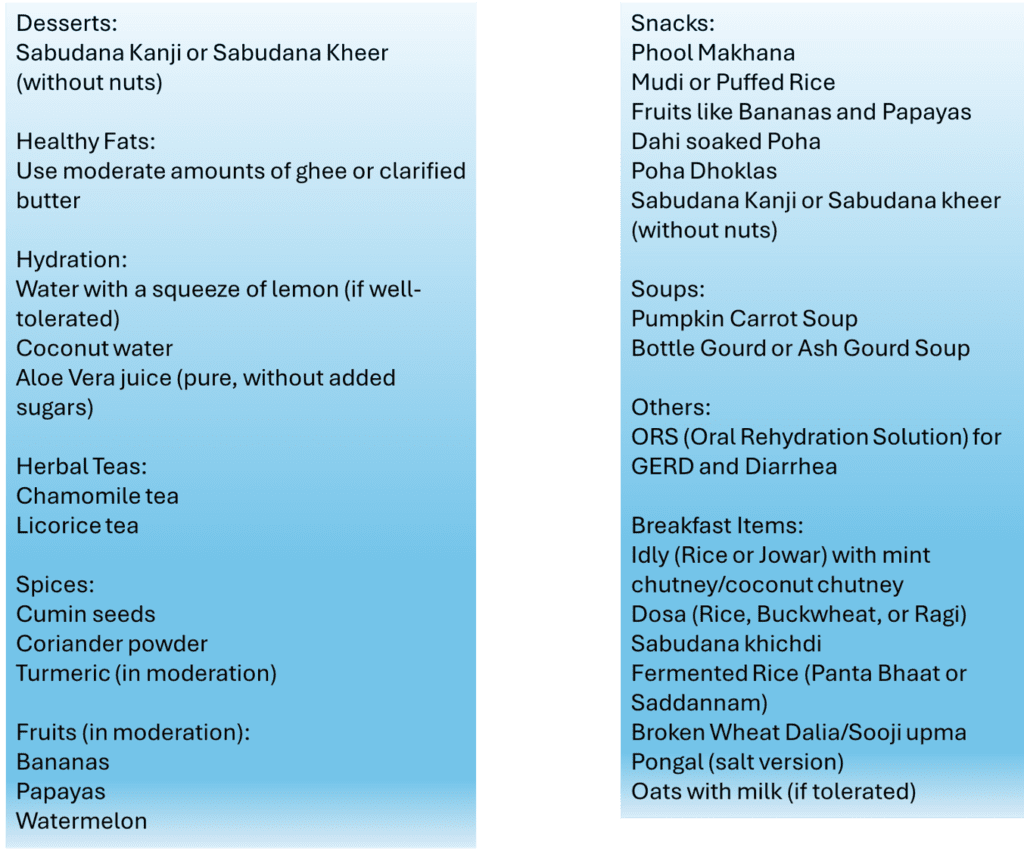
In the upcoming third and fourth weeks, transition to a diet centered around home-cooked, mild foods. Consider the following options for breakfast, meals, and snacks that are gentle on acidity and indigestion during this period.
To manage acidity in an Indian diet, it’s advisable to avoid:
- Spicy Foods: Limit chili peppers and masalas.
- Citrus Fruits: Reduce intake of oranges, lemons, and grapefruits.
- Tomatoes and Tomato-based Products: Minimize tomato consumption.
- Onions and Garlic: Use them sparingly.
- Fried and Fatty Foods: Avoid deep-fried and high-trans fat foods.
- Carbonated Drinks: Steer clear of colas and carbonated beverages.
- Caffeinated Beverages: Limit coffee and strong tea.
- Chocolate: Reduce chocolate with high cocoa content.
- Mint: Minimize use of mint and mint-flavored products.
- Alcohol: Reduce or eliminate alcohol consumption.
- Pickles: Limit acidic pickles.
- Spicy Snacks: Avoid chaat, samosas, and bhel puri.
- Sour Cream: Reduce use in dishes.
- Processed Foods: Limit packaged foods with additives.
- High-fat Dairy: Cut back on full-fat milk, cheese, and creamy desserts.
- Red Meat: Reduce intake for easier digestion.
- Vinegar: Avoid foods high in vinegar content.
- Deep-fried Snacks: Steer clear of samosas and pakoras.
- Excessive Salt: Moderate salt intake.
Individual responses vary, so observe triggers and consult healthcare professionals for personalized advice.
Maintaining a well-balanced diet involves strategic portion control and opting for lighter cooking methods, favoring minimal oil. Prioritize non-spicy meals and ensure optimal hydration with 3 liters (8-10 glasses) of water daily. Jumpstart your day by reaping the benefits of soaked black raisins and prunes (4-5 each) on an empty stomach. Tackle acidity and heartburn by incorporating 1 teaspoon of gulkand with 2 teaspoons of milk into your nightly routine, either between meals or before bedtime.
Infuse freshness into your mornings with a revitalizing cup of Ajwain or Saunf water. Boil a teaspoon of these seeds in 2 cups of water, let it reduce by half, and enjoy sipping throughout the day. Post meals, cleanse your palate with a few mint leaves. Counteract post-dinner acidity by embracing half a teaspoon of jaggery paired with ajwain or saunf. Elevate your post-meal experience with a homemade mukhawas blend. For continued relief from acidity, introduce semi-ripened bananas or steamed apples on an empty stomach. Opt for a healthier routine by excluding coffee, tea, biscuits, and deep-fried snacks.
Week 5:
Should you experience improvement by the conclusion of the fourth week, you may transition to the plan outlined for weeks 5. In the event that symptoms persist, consider extending the current week’s plan for an additional week.
Entering this week, many relish the unhurried pace of their meals, reveling in a heightened awareness of their dietary choices. You might sense a newfound lightness and well-being.
As you enter the 5th week, it’s time to reintroduce certain foods eliminated in the past two weeks. Take it one food at a time, in modest amounts, and diligently record any associated symptoms. This deliberate approach helps discern the nuances of what, when, and how much to consume. By the conclusion of this phase, you’ll likely pinpoint the dietary culprits triggering your digestive concerns. As you craft a modified diet plan, incorporate foods that fortify gut health.
If you find relief with one or two food exclusions, your symptoms may significantly improve within the timeframe of this plan. For those grappling with multiple triggers, allocating an additional 2-3 weeks may be help in identifying and resolving the issues.
Probiotics may help the cause
Probiotics offer a multitude of health benefits, with a key focus on maintaining a robust digestive system. The prolonged use of Proton Pump Inhibitors (PPIs) and antacids disrupts the growth of healthy bacteria and disturbs the natural pH balance in the gut.
While these medications are often prescribed to alleviate symptoms of acidity and indigestion, it’s crucial to address the root cause rather than merely treating symptoms. Probiotics, tiny micro-organisms, play a pivotal role in addressing acidity and indigestion from its core. In the absence of healthy bacteria in the gut, the digestive process slows down, creating an environment conducive to the rapid multiplication of harmful bacteria. Small Intestine Bacterial Overgrowth (SIBO) occurs when these bacteria extend into the small intestine, causing undesirable symptoms such as gas, abdominal pressure, weakened lower esophageal sphincter, and acid reflux. Lactobacillus acidophilus stands out as a proven probiotic for treating acidity and indigestion. Indian culinary offerings like curd, buttermilk, fermented milk drinks, rice, dosa, dhokla, and pickled vegetables such as amla, carrots, radish, cucumbers, along with cheese, serve as excellent sources of probiotics.
Embracing a healthy lifestyle plays a pivotal role in addressing acidity and indigestion, complementing dietary adjustments. Consider these guidelines to manage GERD/Acidity and Dyspepsia/Indigestion effectively.
References:
- Harvard Health Publishing. “9 at-home treatments for acid reflux.”
- National Institute of Diabetes and Digestive and Kidney Diseases. “Symptoms & causes of GER & GERD.”
- National Institute of Diabetes and Digestive and Kidney Diseases. “Definition & facts for GER & GERD.”
- Katz PO, Dunbar KB, Schnoll-Sussman FH, Greer KB, Yadlapati R, Spechler SJ. (2022) “ACG clinical guideline for the diagnosis and management of gastroesophageal reflux disease.” American Journal of Gastroenterology.