What is Crohn’s disease?
Crohn’s disease is a chronic disease that causes inflammation and irritation in the digestive tract. Most commonly, Crohn’s affects the small intestine and the beginning of the large intestine. However, the disease can affect any part of the digestive tract, from the mouth to the anus. Crohn’s disease is an inflammatory bowel disease (IBD). Ulcerative colitis and microscopic colitis are other common types of IBD. Crohn’s disease most often begins gradually and can become worse over time, with periods of remission that can last for weeks or years.
What causes Crohn’s disease?
Experts think the following factors may play a role in causing Crohn’s disease.
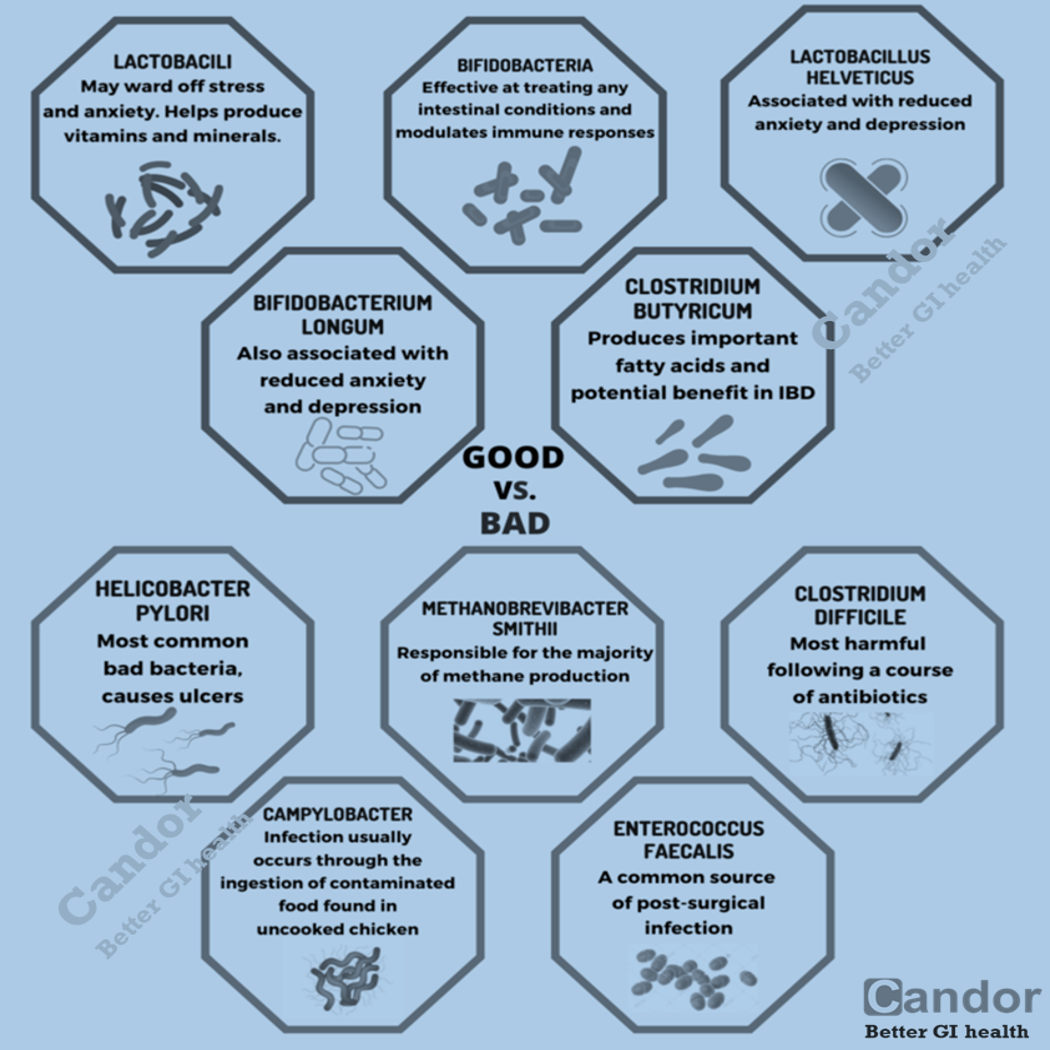
- Autoimmune reaction: One cause of Crohn’s disease may be an autoimmune reaction – when the immune system attacks healthy cells in the body. Experts think bacteria in the digestive tract can mistakenly trigger an immune system response. This immune system response causes inflammation, leading to symptoms of Crohn’s disease.
- Genes: Crohn’s disease sometimes runs in families. Experts continue to study the link between genes and Crohn’s disease.
Some studies suggest that other factors may increase the chance of developing Crohn’s disease:
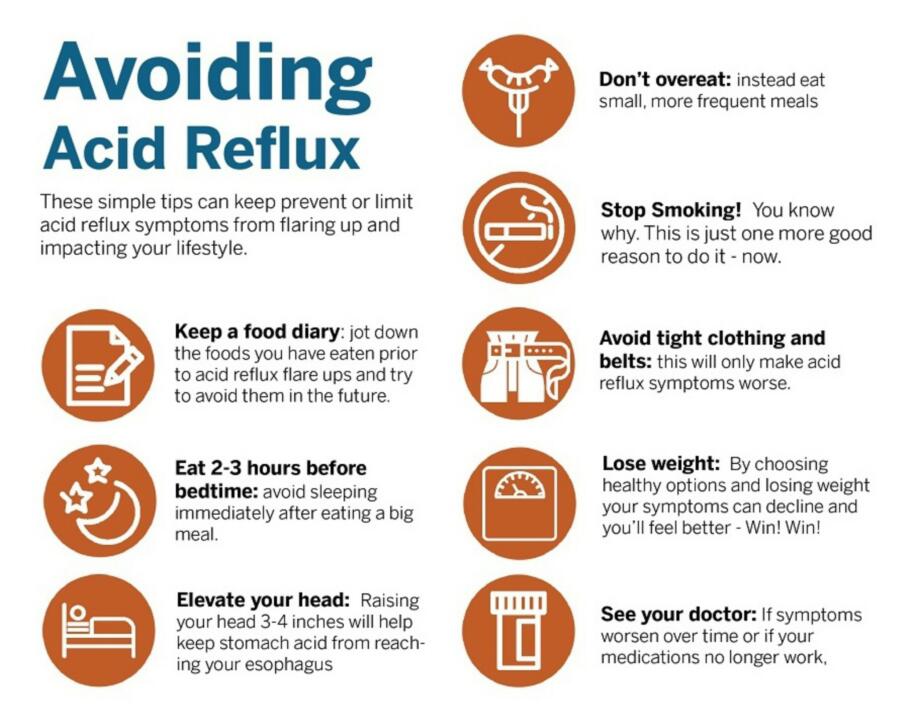
- Smoking may double chances of developing Crohn’s disease.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin or ibuprofen, antibiotics
- A high-fat diet
What are the typical treatment paths for Crohn’s?
- Aminosalicylates: These include medications that contain 5-aminosalicylic acid (5-ASA), and work by inhibiting certain pathways that produce substances that cause inflammation. They can work in the lining of the GI tract to decrease inflammation. They are thought to be effective in treating mild-to-moderate flares of Crohn’s disease, and work best in the colon.
- Corticosteroids: These medications affect the body’s ability to launch and maintain an inflammatory process, and work to keep the immune system in check. Corticosteroids are used in people with moderate to severe Crohn’s disease. Corticosteroids are effective for short-term control of disease activity and are not recommended for long-term use due to associated side effects.
- Immunomodulators: This class of medications controls or suppresses the body’s immune system response, therefore decreasing inflammatory activity. Immunomodulators are generally used when aminosalicylates have not worked well. Some immunomodulators are added to make other medications, such as biologics, work better by preventing the antibody formation to biologic medications. They may be useful in reducing or eliminating the need for corticosteroids, and may also be effective in maintaining remission in people who haven’t responded to other medications.
- Biologic therapies: These are protein-based therapies made from living organisms, and are antibodies that stop certain proteins in the body from causing inflammation. They are currently offered in injectable form, or through intravenous infusion. Biosimilars (similar, near identical copies of another already approved biologic therapy) can have the same safety and effectiveness, and are taken in the same way as the originator drugs.
- Antibiotics: Antibiotics may be used when infections such as abscesses occur in Crohn’s disease. They can also be helpful with fistulas around the anal canal and vagina.
What is ulcerative colitis?
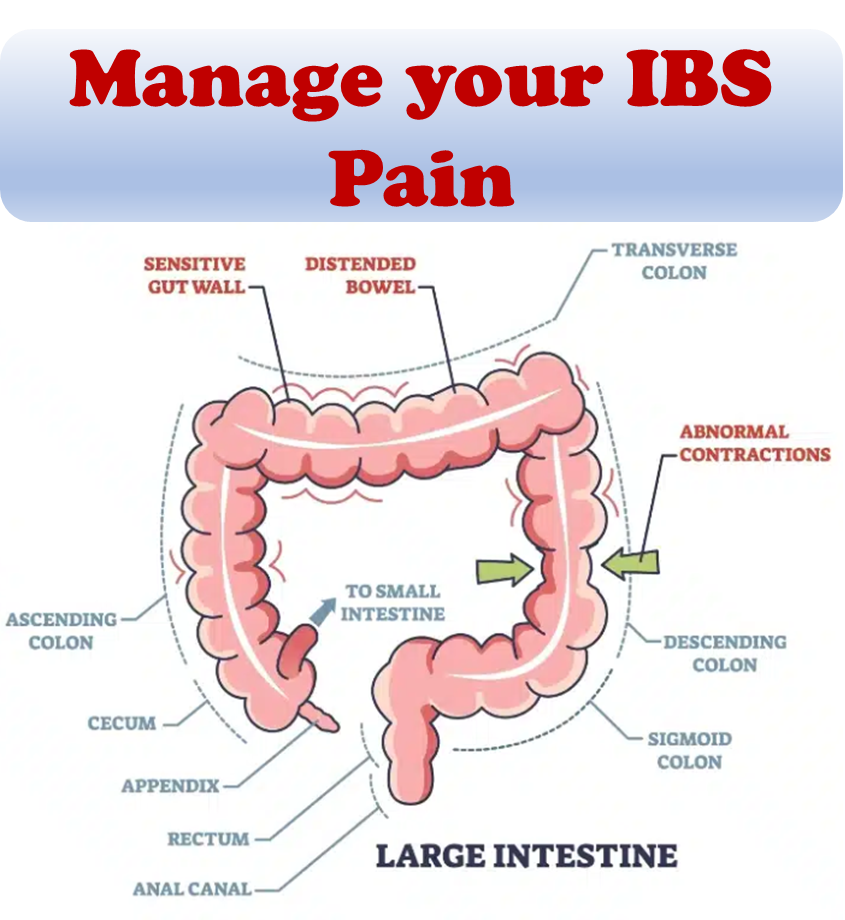
Ulcerative colitis is a chronic inflammatory disease of the gastrointestinal (GI) tract, called inflammatory bowel disease (IBD). Crohn’s disease and microscopic colitis are the other common IBDs. Ulcerative colitis is a chronic disease that causes inflammation and ulcers on the inner lining of the large intestine. Ulcerative colitis most often begins gradually and can become worse over time. Symptoms can be mild to severe. Most people have periods of remission and the goal of care is to keep people in remission long term.
What causes ulcerative colitis?
While the exact cause of ulcerative colitis is unknown, researchers believe the following factors may play a role:
- Overactive intestinal immune system: Normally, the immune system protects the body from infection by identifying and destroying bacteria, viruses, and other potentially harmful foreign substances. Researchers believe bacteria or viruses can mistakenly trigger the immune system to attack the inner lining of the large intestine. This immune system response causes the inflammation, leading to symptoms.
- Genes: Research studies have shown that certain abnormal genes may run in families and appear in people with ulcerative colitis. However, researchers have not been able to show a clear link between the abnormal genes and ulcerative colitis.
- Environment: Some studies suggest that certain things in the environment may increase the chance of a person getting ulcerative colitis, although the overall chance is low. Nonsteroidal anti-inflammatory drugs, antibiotics, and oral contraceptives may slightly increase the chance of developing ulcerative colitis. A high-fat diet may also slightly increase the chance of getting ulcerative colitis.
- Stress and diet: Some people believe eating certain foods, stress, or emotional distress can cause ulcerative colitis. A few studies suggest that stress may increase a person’s chance of having a flare-up of ulcerative colitis. Also, some people may find that certain foods can trigger or worsen symptoms.
Types of Ulcerative Colitis
- Ulcerative Proctitis: Bowel inflammation is limited to the rectum (usually less than six inches of the rectum) and is not associated with an increased risk of cancer. Symptoms include rectal bleeding, urgency, and rectal pain. This form of ulcerative colitis tends to be the mildest.
- Left-sided Colitis: Inflammation extends from the rectum up through the sigmoid and descending colon. Signs and symptoms include bloody diarrhea, abdominal cramping and pain on the left side, and unintended weight loss.
- Proctosigmoiditis: Inflammation involves the rectum and sigmoid colon (lower end of the colon). Signs and symptoms include bloody diarrhea, abdominal cramps and pain, and an inability to move the bowels in spite of the urge to do so (tenesmus).
- Pancolitis: Often affects the entire colon, with bouts of bloody diarrhea that may be severe. Other symptoms include loss of appetite, abdominal pain, fatigue and weight loss.
Incidence patterns for Crohn’s vs Colitis
IBD is widely believed to be associated with industrialization of nations. This hypothesis is supported by the significant geographic variation in IBD with the highest incidence rate of IBD in North America and Europe. The number of cases of IBD is increasing in China, India, and South America.
Both Crohn’s disease and ulcerative colitis are found mainly in developed countries, in urban areas and northern climates. Crohn’s disease can occur at any age, although on average, people are most frequently diagnosed between 20 and 30. Males and females appear to have similar statistics on prevalence. Pediatric Crohn’s disease has also been reported to be on the rise globally. It tends to be more common among Caucasians, but prevalence and incidence rates among Hispanics and Asians is on the rise. While the incidence and prevalence rates of Crohn’s disease have been increasing rapidly, and the disease is no longer uncommon in Asian and developing countries, these rates are still lower than those in developed countries.
Crohn’s vs Colitis
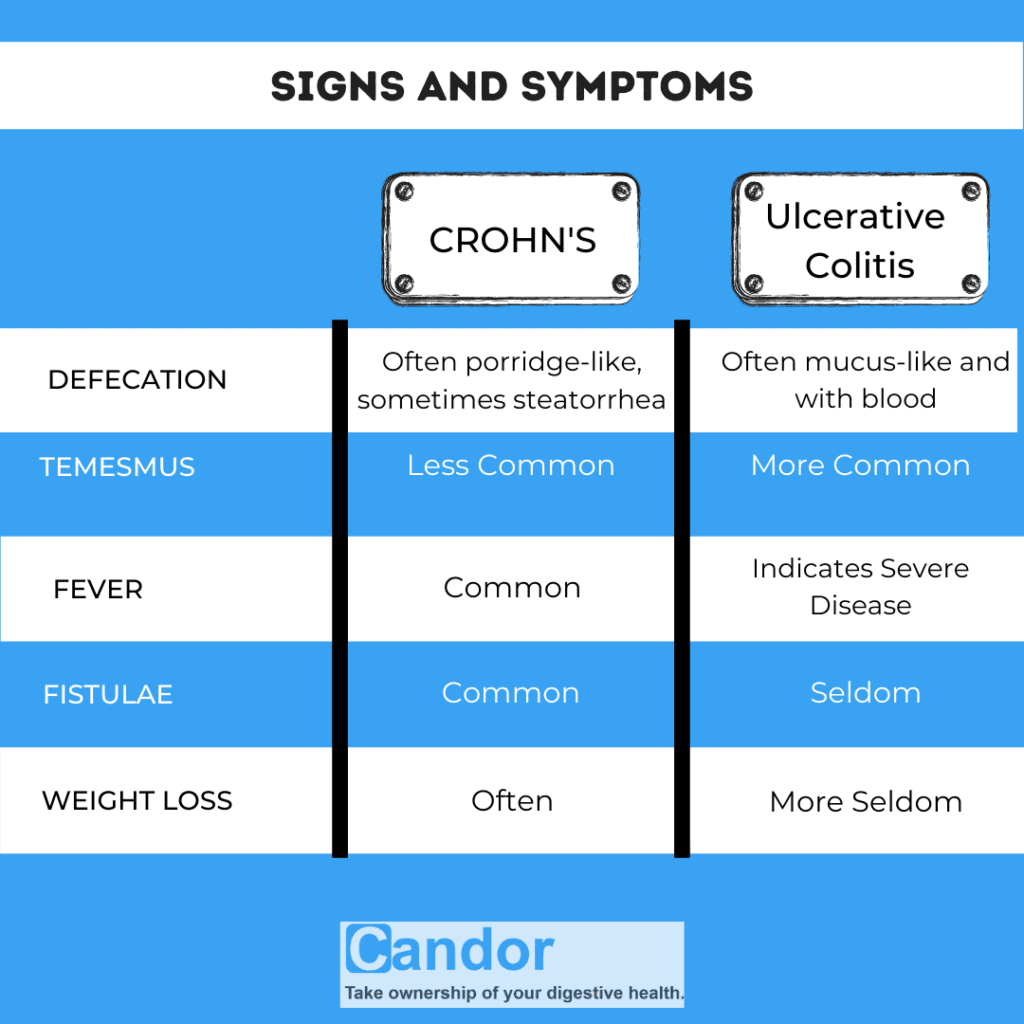
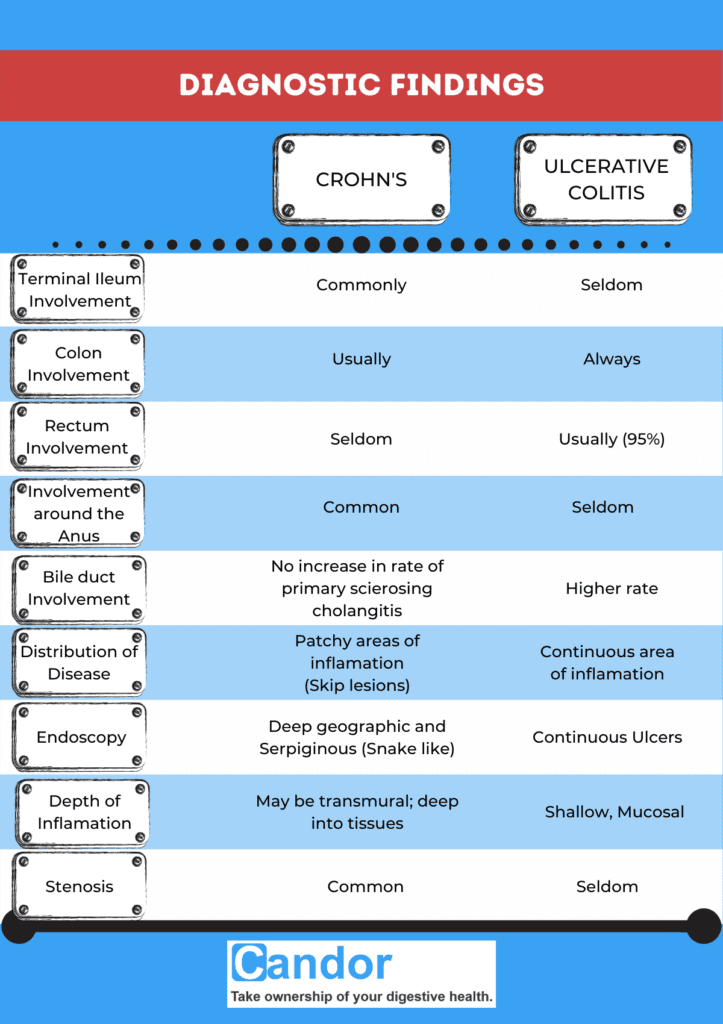
In spite of Crohn’s and Ulcerative Colitis being very different diseases, both may present with any of the following symptoms: abdominal pain, diarrhea, rectal bleeding, severe internal cramps/muscle spasms in the region of the pelvis and weight loss.
Anemia is the most prevalent extraintestinal complication of inflammatory bowel disease. Diagnosis is generally by assessment of inflammatory markers in stool followed by colonoscopy with biopsy of pathological lesions.
Crohn’s disease can affect any part of the GI tract from the mouth to the anus and can affect the entire thickness of the bowel wall. In Ulcerative Colitis, only the colon and rectum are affected and also affects the inner-most lining of the large intestine.
References:
- Hovde Ø, Moum BA (April 2012). “Epidemiology and clinical course of Crohn’s disease: results from observational studies”. World Journal of Gastroenterology.
- Yamamoto-Furusho JK, Korzenik JR (November 2006). “Crohn’s disease: innate immunodeficiency?”. World Journal of Gastroenterology.
- Hanauer SB, Sandborn W (March 2001). “Management of Crohn’s disease in adults”. The American Journal of Gastroenterology.
- “What I need to know about Crohn’s Disease”. www.niddk.nih.gov.
- Akiho H, Yokoyama A, Abe S, Nakazono Y, Murakami M, Otsuka Y, et al. (November 2015). “Promising biological therapies for ulcerative colitis: A review of the literature”. World Journal of Gastrointestinal Pathophysiology.
- Danese S, Fiocchi C (November 2011). “Ulcerative colitis”. The New England Journal of Medicine.
- Vos, Theo; et al. (GBD 2015 Disease and Injury Incidence and Prevalence Collaborators) (October 2016). “Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015”. Lancet.