As we age, our immune system undergoes significant changes, adapting to maintain a delicate balance between defense and tolerance. This intricate process allows it to effectively combat harmful invaders while distinguishing and tolerating our own cells and tissues. Various factors, such as proteins in maternal milk and the influence of sex hormones, contribute to establishing this equilibrium.
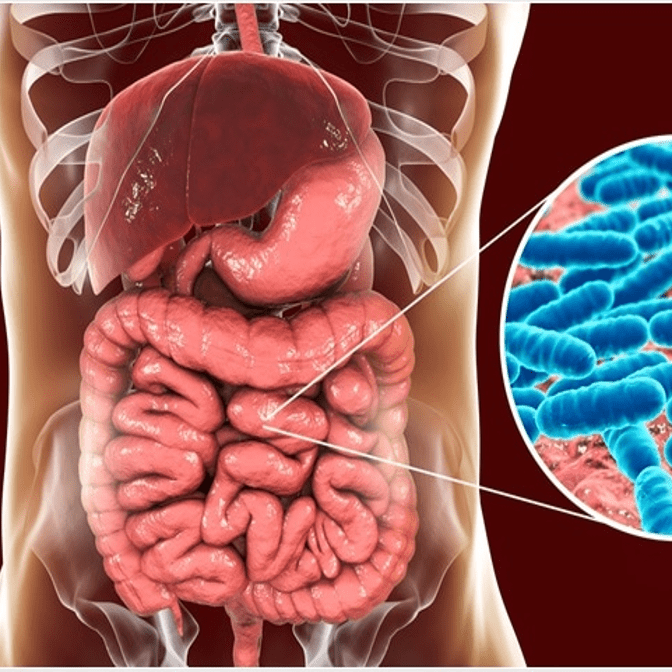
In recent years, scientific interest has turned towards the role of gut bacteria, a crucial influencer in shaping our immune responses. Despite the growing attention on the human microbiome, there remains much to uncover about how the myriad of microscopic passengers within us influence our immune system’s functionality.
The role of gut bacteria is to help normal functioning of the gastrointestinal tract and any imbalance can lead to potential discomfort during digestion. There is a growing body of evidence indicating their complex role in a number of GI disorders including IBS. It is unclear whether the alterations in bacterial flora are a cause or a consequence of the disorder.
If you want to know more about the different kinds of gut bacteria, check out this article.
People with IBS appear to have an altered composition of GI bacteria, specifically a reduction in diversity of bacterial species and an overabundance of some bacterial species. GI bacteria responsible for fermentation of poorly absorbed fermentable carbohydrates may be altered in people with IBS resulting in looser stools and increased gas production. GI bacteria may also play a role in gut motility and the perception of pain due to factors such as stimulation of smooth muscle and bile acid malabsorption.
IBS is also characterized by increased mucosal immune responses due to loss in function of the bowel epithelial barrier could lead to and implies IBS is similar to a milder form of Inflammatory Bowel Disease (IBD), a digestive illness which is characterized by visible changes in the digestive tract. Crohn’s disease is an inflammatory disorder that impacts the digestive tract, often resulting in persistent pain, nutritional deficiencies, and in severe cases, life-threatening complications. Psoriasis is characterized by skin rashes and, at times, inflamed joints. On the other hand, Type 1 diabetes manifests when the pancreas fails to produce insulin, affecting the body’s ability to utilize sugar for energy. Despite their unique presentations, these conditions share a crucial similarity—they are believed to stem from dysfunctional T-cells.
T-cells originate within the bone marrow and undergo a complex transformation within a small gland located between the lungs before taking on various roles within the immune system. For instance, Th17 cells are aggressive in their response, releasing pro-inflammatory signals to rally other immune cells and combat pathogens. In contrast, regulatory T-cells act as moderators, slowing down immune responses when they are unnecessary.
Disruption of T-cell balance between the types can lead to severe consequences. For instance, in psoriasis, T-cells erroneously attack skin cells, causing a range of symptoms. Inflammatory bowel diseases (IBD) such as Crohn’s disease and ulcerative colitis are characterized by uncontrolled immune responses that damage the digestive tract. Moreover, T-cell dysfunction is implicated in other chronic conditions like multiple sclerosis and rheumatoid arthritis. Understanding how to regulate T-cell activity has become a crucial medical inquiry. Recent advancements have shed light on the potential role of bacteria in influencing T-cell behavior, opening new avenues for research and treatment.
References:
- Moszak, M; Szulińska, M; Bogdański, P (15 April 2020). “You Are What You Eat-The Relationship between Diet, Microbiota, and Metabolic Disorders-A Review”. Nutrients. 12 (4): 1096.
- Saxena, R.; Sharma, V.K (2016). “A Metagenomic Insight Into the Human Microbiome: Its Implications in Health and Disease”.
- Shen, Sj; Wong, Connie HY (2016). “Bugging inflammation: Role of the gut microbiota”. Clinical & Translational Immunology. 5 (4): e72.
- Khanna, Sahil; Tosh, Pritish K (2014). “A Clinician’s Primer on the Role of the Microbiome in Human Health and Disease”.



























