You’re probably aware that your body is made up of trillions of cells. These little guys, about 30 trillion of them in an average human, may be tiny, but they play an incredibly important role in keeping your body in tip-top shape. They provide structure, transform nutrients into energy, and carry out specific tasks depending on where they are in your body.
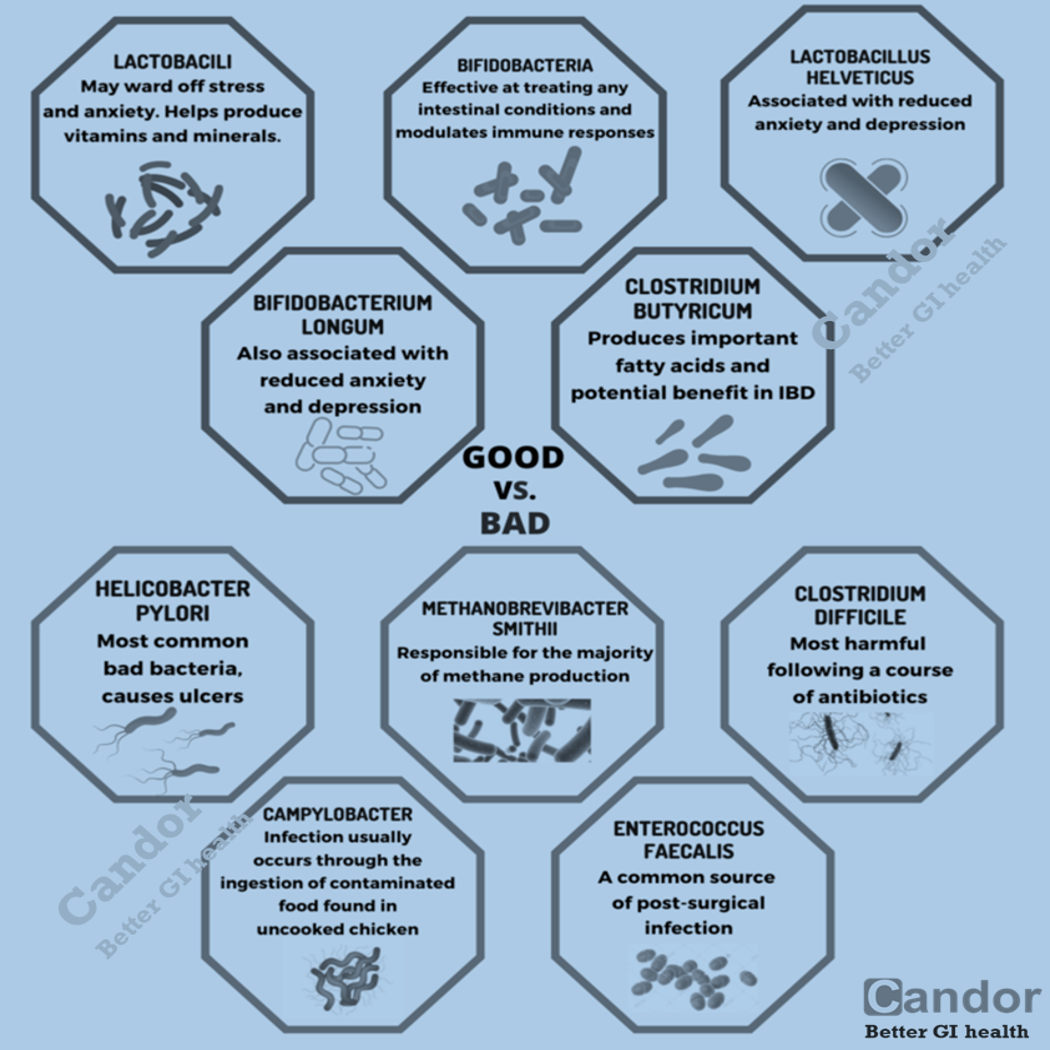
Did you know that not all bacteria are out to get you? It’s a common mistake to assume that every single bacterium is a menace, especially when every cleaning product on the shelf claims to obliterate them. Sure, there are some bacteria that can be troublemakers. They can release toxins that harm your cells and contribute to various diseases. But here’s the thing: not all bacteria are bad for you. In fact, your body relies on some bacteria to keep things running smoothly.
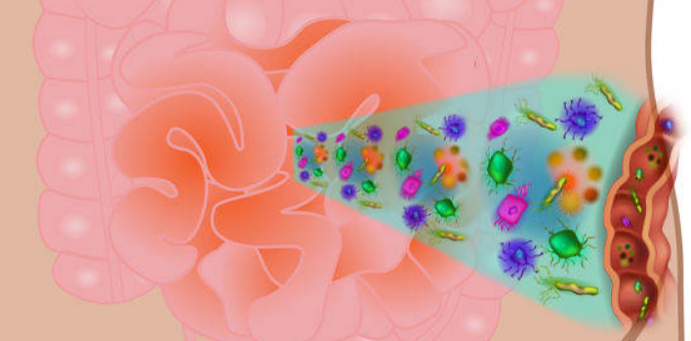
But here’s a fun fact you might not know: your body is also a bustling metropolis for an estimated 39 trillion microbes. That includes bacteria, viruses, and fungi. These microscopic organisms are actually essential for a healthy life because they perform a bunch of vital functions. For instance, your immune system relies on these microbial cells to fend off infections, neutralize toxins, and safeguard the rest of your cells.
And guess what? Your digestive system is in cahoots with friendly bacteria too. That’s why there are so many different types of bacteria species hanging out in your stomach—hundreds of them, in fact. These good bacteria work hard to break down the food you eat, unlocking all those essential nutrients and making them available to the rest of your cells and organs.
Those nutrients are crucial for giving you energy, supporting growth, and repairing your cells. While we owe a lot to the bacteria in our stomachs for helping with digestion, it’s worth noting that too much of a good thing can be a bit problematic.
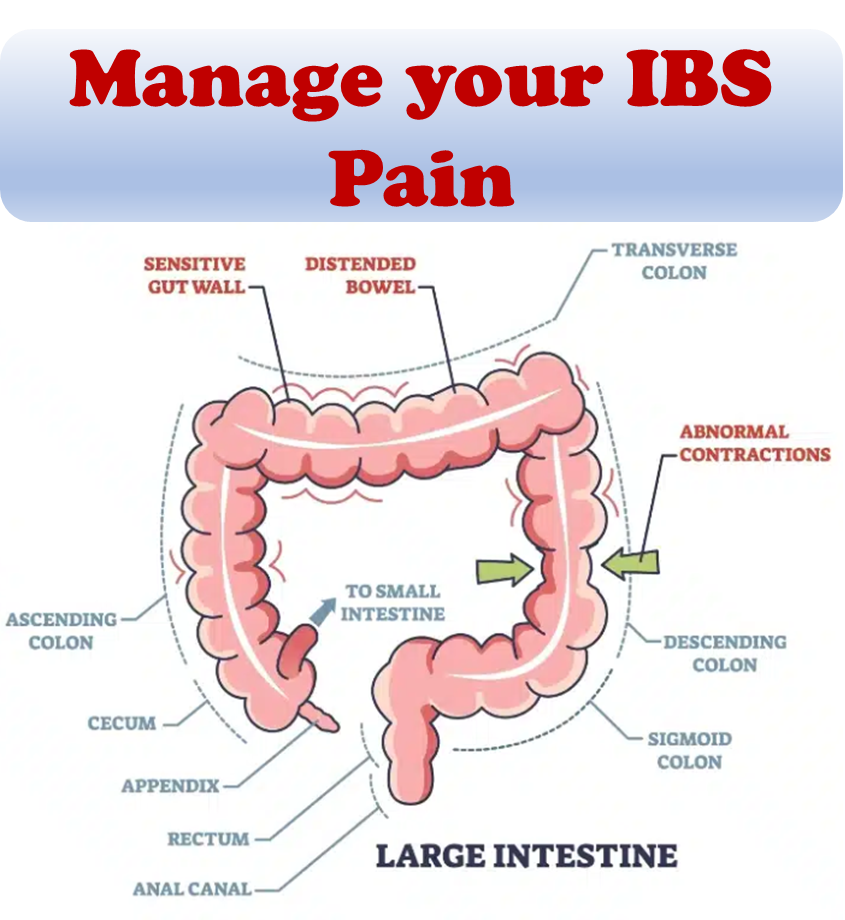
The large intestine, also known as the colon, specifically requires colonic bacteria as an essential component for proper digestion after the small intestine. Nevertheless, when bacteria strays from its designated path and infiltrates the small intestine, it disrupts the delicate equilibrium of your digestive system, potentially leading to an imbalance. See our article on SIBO.
SIBO, short for small intestinal bacterial overgrowth, occurs when there is an excessive presence of colonic bacteria in the small intestine, deviating from its normal state. Every section of the digestive system relies on distinct bacteria to carry out vital functions.
Unraveling the origins of SIBO: understanding its causes
The human body diligently maintains the equilibrium of its microbiome, the intricate ecosystem of bacteria, through a myriad of intricate chemical and mechanical processes. However, a malfunction in any of these systems can disrupt the natural flow, leading to a buildup of food and waste products within the small intestine. This, in turn, creates an inviting environment for the proliferation of undesirable bacterial strains, ultimately giving rise to the condition known as SIBO.
Within the small intestine, a delicate interplay of chemicals assumes the responsibility of degrading and breaking down food. The harmonious presence of bile, enzymes, immunoglobulin, and gastric acid stands paramount in maintaining a favorable balance of bacteria. However, certain medical conditions, gastric bypass surgery, and the administration of specific medications can impede the synthesis and efficacy of these vital chemicals, rendering the small intestine bacteria ill-equipped to fulfill their role of food degradation.
In addition to chemical processes, the mechanical functioning of the small intestine plays a crucial role. Its inherent task is to expel its contents into the expansive confines of the large intestine upon completing its duties. Yet, obstructions, twists, or hernias can impede this essential cleansing mechanism, preventing prompt and efficient evacuation.
As food remnants and waste products accumulate within the small intestine, an unwelcome consequence emerges—the infiltration of colonic bacteria into this delicate domain. This unwarranted intrusion further fuels the development of SIBO, exacerbating the imbalance and its associated complications.
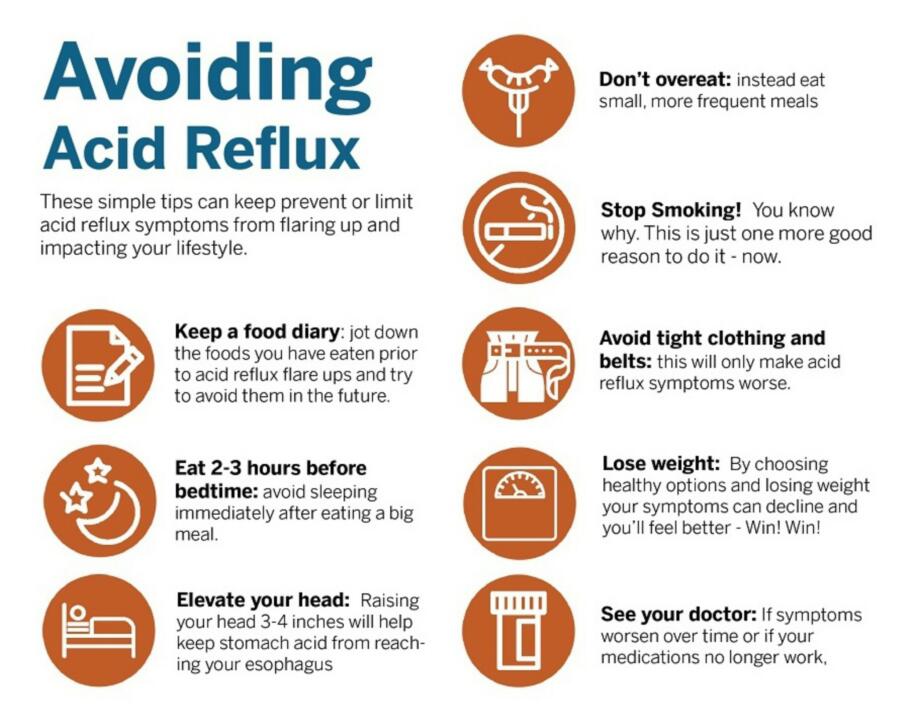
Typically, a blend of prescription antibiotics is employed to tackle SIBO cases. However, the challenge lies in the frequent recurrence of SIBO following antibiotic treatment. The reoccurrence of SIBO is particularly common when there exists an underlying predisposition. Therefore, it is generally recommended to adopt certain lifestyle modifications that can mitigate the intensity and probability of SIBO occurrences.
SIBO Natural remedies for respite from symptoms
- Low-FODMAP diet: taming bacterial fuel
An alternative to the keto diet, the low-FODMAP diet targets non-digestible and short-chain sugars that stimulate bacterial growth. FODMAP, an acronym for “fermentable oligosaccharides, disaccharides, monosaccharides, and polyols,” guides the elimination of specific foods rich in these substances. - Elemental diet: nourishing the body, starving the bacteria
To combat SIBO, a strategic approach involves providing essential nutrients while depriving the bacteria in the small intestine. The elemental diet offers a solution by excluding dietary fiber, probiotics, plant and animal proteins, and gluten. Predigested liquid formulas ensure optimal nutrient intake without reliance on gut bacteria for extraction. Although recommended for a limited duration, the elemental diet serves as a crucial initial step in SIBO treatment. - Keto diet: reducing carbohydrate fuel for bacteria
As bacteria thrive on carbohydrates, limiting their growth becomes paramount in SIBO management. The ketogenic diet emphasizes the replacement of carbs with healthy fats, significantly reducing carbohydrate intake. While carbohydrates are not entirely eliminated, the target is to consume less than 20 grams per day. - MCTs: embracing healthy fats
Medium-chain triglycerides (MCTs), found in coconut oil, palm kernel oil, and select dairy products, offer numerous benefits for the body and brain. MCTs are directly absorbed without the need for digestive enzymes, making them beneficial in SIBO management. - Nutrient supplements: replenishing essential elements
SIBO often leads to nutrient deficiencies, hindering proper functioning and absorption in the small intestine. Vitamin deficiencies, such as A, B12, D, E, and K, and mineral deficiencies, including calcium, copper, iron, magnesium, and zinc, require attention through targeted supplementation. - Digestive enzymes: enhancing digestion and nutrient absorption
Supplementing with digestive enzymes aids in treating SIBO by alleviating symptoms, improving nutrient absorption, and expanding the range of tolerated foods. Protease breaks down proteins, lipase targets fats, and amylase aids in carbohydrate digestion. - Natural probiotics: balancing the microbial landscape
Although seemingly contradictory, certain probiotics can aid in managing bacterial overgrowth by replacing harmful bacteria and promoting a healthier digestive tract. Consider incorporating probiotics such as Bacillus indicus, Lactobacillus plantarum, Saccharomyces boulardii, Lactobacillus GG, Bigodbactermimum infantis 35624, Lactobacillus casei, and Bifidus lactis. - Herbal therapy: tapping into nature’s antibacterial arsenal
Harnessing the therapeutic properties of herbs can effectively alleviate SIBO symptoms. Herbal supplements with potent antimicrobial qualities play a crucial role in eradicating bacterial overgrowth. Combining various herbal supplements over a few months facilitates comprehensive treatment. Some notable herbs include allicin, ayurveda, barberry, berberine, clover or clove oil, coptis chinensis, goldenseal, grapefruit seed extract, neem extract, olive leaf extract, oregon grape root, oregano leaf or oil, pau d’arco, peppermint oil, phildendriod, pomegranate husk, propolis, and thyme oil.
By exploring these natural remedies, individuals can augment their SIBO treatment approach, empowering their bodies to combat bacterial overgrowth and restore digestive balance.
In conclusion: managing SIBO and finding relief
Living with SIBO can be a distressing experience, and often, symptoms may arise long after the condition has taken hold. If you find yourself frequently or severely experiencing SIBO symptoms, it is advisable to consult a healthcare professional who can diagnose any underlying causes and suggest appropriate treatment options.
While complete eradication of SIBO may not always be feasible, there are several strategies that can bring relief. Utilizing a holistic approach involving a blend of herbs, enzymes, medium-chain triglycerides (MCTs), nutrient supplements, and probiotics, alongside the avoidance of SIBO-triggering foods, can help alleviate symptoms and maintain a semblance of control over the condition.
Remember, finding the right combination of approaches and making necessary lifestyle modifications can go a long way in managing SIBO and reducing its impact on your daily life.
References:
- Bures J, Cyrany J, Kohoutova D, Förstl M, Rejchrt S, Kvetina J, et al. (June 2010). “Small intestinal bacterial overgrowth syndrome”. World Journal of Gastroenterology.
- Quigley E, Murray J, Pimentel M (October 2020). “AGA Clinical Practice Update on Small Intestinal Bacterial Overgrowth: Expert Review”. Gastroenterology.
- Sachdev AH, Pimentel M (September 2013). “Gastrointestinal bacterial overgrowth: pathogenesis and clinical significance”. Therapeutic Advances in Chronic Disease.
- Ford AC, Spiegel BM, Talley NJ, Moayyedi P (December 2009). “Small intestinal bacterial overgrowth in irritable bowel syndrome: systematic review and meta-analysis”. Clinical Gastroenterology and Hepatology.
- Dukowicz AC, Lacy BE, Levine GM (February 2007). “Small intestinal bacterial overgrowth: a comprehensive review”. Gastroenterology & Hepatology.
- Meier R, Burri E, Steuerwald M (September 2003). “The role of nutrition in diarrhoea syndromes”. Current Opinion in Clinical Nutrition and Metabolic Care.
- Bested AC, Logan AC, Selhub EM (March 2013). “Intestinal microbiota, probiotics and mental health: from Metchnikoff to modern advances: part III – convergence toward clinical trials”. Gut Pathogens.