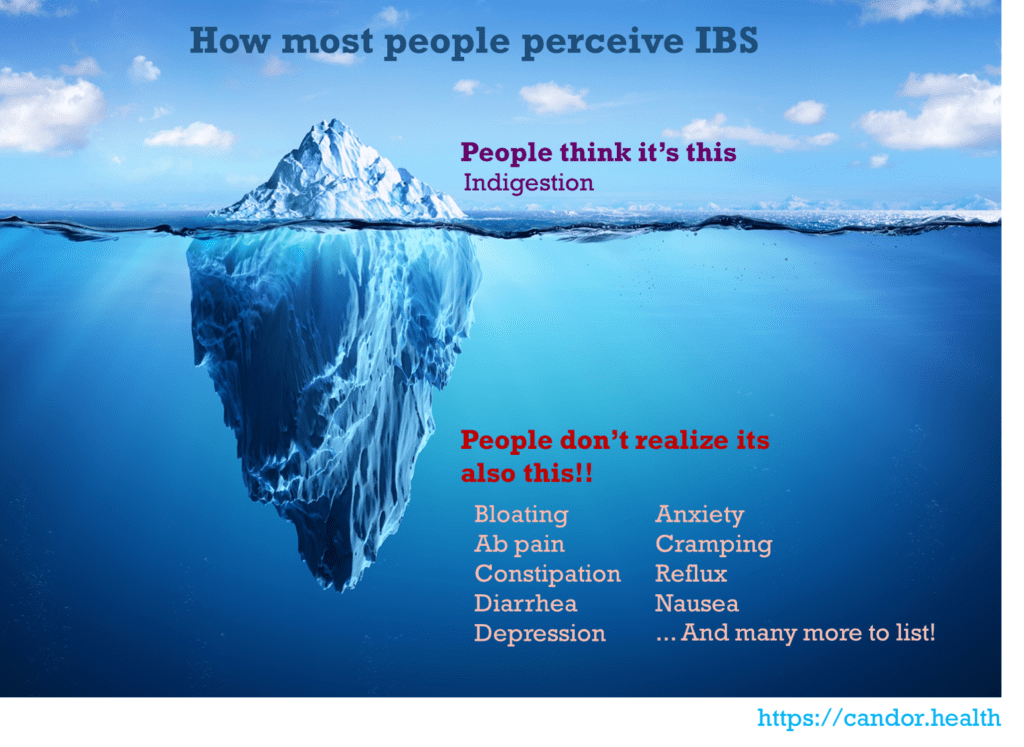
Irritable bowel syndrome (IBS) affects a staggering number of individuals, with estimates ranging from 25 to 45 million in the United States alone. Surprisingly, this condition, which affects approximately 5% to 10% of the global population, is still not taken as seriously as it should be. To those who have never experienced it, IBS may seem like a mere bout of indigestion, easily brushed aside. However, for those living with IBS, it can consume their entire existence, revolving around chronic abdominal pain, bloating, diarrhea, constipation, or a combination of these symptoms.
Within this realm of IBS, a relentless cycle emerges. People find themselves meticulously avoiding trigger foods, social gatherings involving food and drinks (which encompasses nearly every social event), and any situation that lacks proximity to a bathroom. Only those who endure this condition truly comprehend the realities of living with IBS.
Here are a few of the things people don’t realize about IBS:
- The mental and gastrointestinal turmoil of socializing
The frustration of others failing to comprehend the urgency of immediate bathroom needs, the anxiety of dating while needing frequent restroom visits, and the awkwardness of abruptly dashing off mid-enjoyment—all these stem from visceral hypersensitivity. This phenomenon refers to the experience of pain or discomfort originating from internal organs, occurring under circumstances that would typically be painless, such as eating or during a bowel movement. The gut-brain connection transmits these sensations to the brain, resulting in moments when a meal or fluid intake sends an urgent signal to the colon, completely disregarding one’s conversational flow during a first date. - The comfort found within the confines of home
For those with IBS, the ability to work from home provides a profound sense of relief. Being able to eat intuitively and having immediate access to a nearby bathroom can alleviate anxiety and facilitate a more relaxed experience. However, leaving the comfort of one’s familiar environment can quickly trigger uncertainty and anxiety, heightening the vigilance towards potential symptoms outside the home. - The persistence of dismissive diagnoses
Receiving a diagnosis of IBS can be challenging, as there is no specific biomarker for the condition. Physicians rely on the Rome IV criteria, which take into account specific symptoms and the absence of other alarming indicators. Unfortunately, individuals with IBS often encounter disbelief or dismissive attitudes, leaving them frustrated and unheard, with their symptoms wrongly attributed to psychological factors. - The paradoxical worry that manifests physical distress
The mind-body connection plays a significant role in IBS. When consumed by stress regarding our gut health, the anticipation of symptom exacerbation can actually trigger physical responses within our digestive system. Consequently, we experience tightened abdominal muscles, colon spasms, and increased discomfort. - The immediate toll of impulsive eating or drinking
IBS sufferers must navigate the hyper-responsiveness of the enteric nervous system, the intricate network within our digestive tract. Unpredictable symptoms frequently accompany IBS, leaving individuals hesitant to sample new items on a restaurant menu or partake in happy hour cocktails, for fear of triggering an onset of symptoms. Though these precautions may appear excessive to those unfamiliar with IBS, they determine whether one can fully enjoy social interactions or inadvertently spend the majority of their time confined to the bathroom. - The transformation of recipes or food orders into unrecognizable dishes
The average person can largely control the effects of what they consume, adjusting to food-centric situations with relative ease due to their stable and clear-cut food sensitivities. However, IBS frequently involves food intolerances, and even when individuals carefully monitor their diet, visceral hypersensitivity and disrupted gut-brain communication can lead to unexpected flare-ups. Despite altering ingredients in recipes or food orders to an extensive degree, the resulting meal often bears little resemblance to the original. - The preemptive mapping of public restrooms
The incessant activity of the gut leads to the brain typically filtering out the nerve signals it receives. It selectively attends to certain signals to regulate gut activity while disregarding others. However, prolonged disturbances to the nervous system or the brain—such as during travel, high-stress jobs, or rushed errands—can disrupt normal gut-brain communication. As a result, meticulously plotting the locations of public restrooms becomes a necessity before venturing outside. - The repertoire of bathroom break excuses
While eating and having bowel movements are vital for our survival, they are rarely suitable topics for dinner-table conversations, except when toilet training a toddler. IBS sufferers must maintain a repertoire of plausible excuses for frequent bathroom breaks, adding an extra layer of secrecy, diversion, and occasional embarrassment to their daily lives. These circumstances can even lead to disordered eating habits, with individuals intentionally skipping meals to avoid the need for repeated bathroom visits. - The debilitating exhaustion of severe flare-ups
IBS disrupts the normal movement of food, fluid, and waste through the gut, resulting in irregular bowel habits. Flare-ups can be so severe that individuals may find themselves unable to work or attend school, drained both physically and emotionally. The subsequent frustration and exhaustion add to the overwhelming burden, leaving individuals feeling incapacitated.
If you are considering medical treatment, expect lots of tests. IBS is a diagnosis of exclusion, which means that other diseases and infections must be ruled out before it can be diagnosed. Physicians often run several tests to ensure that there is no inflammation, infection, or other disease causing the symptoms. Diagnosing IBS typically involves a physical exam and medical history. Since it is important to exclude other GI conditions, doctors don’t use tests alone to diagnose IBS. The evaluation may include blood tests, stool samples, endoscopic procedures (such as sigmoidoscopy and colonoscopy), or imaging procedures (like a CT scan or MRI).
Unfortunately, all these tests are not free, and can be quite expensive for someone with sub-par insurance coverage.
Don’t believe the miracle diets and shaman cures out there. Low FODMAP, gluten free, probiotics and a myriad other treatments, supplements and diets been touted to be the panacea for IBS and related GI disorders to varying degrees. There is no one solution unfortunately. IBS is individual specific and what works for one person can exacerbate symptoms in another.
IBS does not go away. But it can be managed. Keeping a log of one’s symptoms and foods that aggravate them has been a popular tactic amongst many people suffering from IBS. It requires patience, will power and diligence. But the long-term rewards may be well worth it. One approach is to keep track of food intake and any associated symptoms or flareups for a timeframe (4-6 weeks). At the start, it may make the most sense to start with a limited set of food items and slowly expand the list as time goes on. For example, steamed vegetables, rice and a fruit in week 1.
References:
- “Definition and Facts for Irritable Bowel Syndrome”. NIDDKD. February 23, 2015.
- Chey WD, Kurlander J, Eswaran S (March 2015). “Irritable bowel syndrome: a clinical review”. JAMA.
- Whitehead WE, Palsson O, Jones KR (April 2002). “Systematic review of the comorbidity of irritable bowel syndrome with other disorders: what are the causes and implications?”. Gastroenterology.
- Brenner DM, Moeller MJ, Chey WD, Schoenfeld PS (April 2009). “The utility of probiotics in the treatment of irritable bowel syndrome: a systematic review”. The American Journal of Gastroenterology.
- Drossman DA (February 2016). “Functional Gastrointestinal Disorders: History, Pathophysiology, Clinical Features and Rome IV”.
- Hou JK, Lee D, Lewis J (October 2014). “Diet and inflammatory bowel disease: review of patient-targeted recommendations”. Clinical Gastroenterology and Hepatology (Review).



























