What is Crohn’s disease?
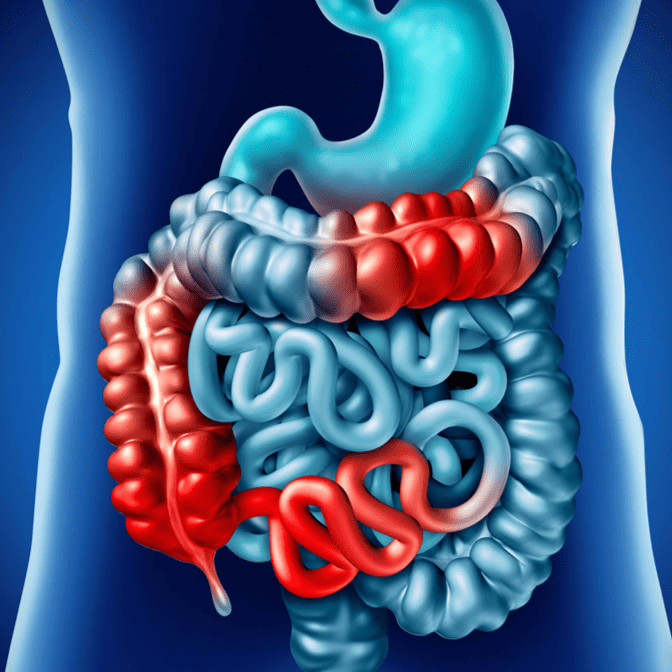
Crohn’s disease is a chronic disease that causes inflammation and irritation in the digestive tract. Most commonly, Crohn’s affects the small intestine and the beginning of the large intestine. However, the disease can affect any part of the digestive tract, from the mouth to the anus. Crohn’s disease is an inflammatory bowel disease (IBD). Ulcerative colitis and microscopic colitis are other common types of IBD. Crohn’s disease most often begins gradually and can become worse over time, with periods of remission that can last for weeks or years.
Crohn’s disease belongs to a category of inflammatory bowel diseases (IBD) characterized by inflammation of the digestive tract. This condition gives rise to various symptoms such as abdominal pain, severe diarrhea, fatigue, weight loss, and malnutrition. The inflammation associated with Crohn’s disease can affect different parts of the digestive tract, with the small intestine being the most commonly affected area. This inflammation often extends into the deeper layers of the intestinal wall. Crohn’s disease can be both distressing and debilitating, and in some cases, it may pose life-threatening complications.
While there is currently no known cure for Crohn’s disease, there are therapies available that can significantly alleviate its symptoms. These treatments can even induce long-term remission and promote the healing of inflammation. With appropriate management, many individuals with Crohn’s disease are able to lead functional and fulfilling lives.
Many individuals with Crohn’s disease endure symptoms for an extended period of time before receiving a diagnosis. While the typical onset of the disease occurs during the teenage and twenties years, it can manifest at any age. Due to the “patchy” nature of this gastrointestinal condition and the depth of tissue affected, initial symptoms may be more subtle compared to those of ulcerative colitis. Crohn’s disease is characterized by recurring periods of flare-ups and remission, leading to chronicity. The symptoms experienced can evolve over time as inflammation progresses and spreads throughout the body. Furthermore, the specific symptoms can vary depending on the organs involved. Given the high variability of symptoms, organ involvement, and initial presentation, it is widely acknowledged that each patient’s experience with Crohn’s disease is unique.
What causes Crohn’s disease?
Experts think the following factors may play a role in causing Crohn’s disease.
- Autoimmune reaction: One cause of Crohn’s disease may be an autoimmune reaction – when the immune system attacks healthy cells in the body. Experts think bacteria in the digestive tract can mistakenly trigger an immune system response. This immune system response causes inflammation, leading to symptoms of Crohn’s disease.
- Genes: Crohn’s disease sometimes runs in families. Experts continue to study the link between genes and Crohn’s disease.
Some studies suggest that other factors may increase the chance of developing Crohn’s disease:
- Smoking may double chances of developing Crohn’s disease.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin or ibuprofen, antibiotics
- A high-fat diet
To understand the incidence patterns of Crohn’s disease, click here.
There is currently no known cure for Crohn’s disease. The primary objective of treatment options is to alleviate symptoms, maintain periods of remission, and prevent relapses. In cases of newly diagnosed individuals, a short-term use of corticosteroids may be prescribed to rapidly improve symptoms. Smoking cessation is strongly recommended for individuals with Crohn’s disease. Hospitalization is necessary for approximately one in five people with the disease each year, and over a ten-year period, half of them will require surgery. While surgical intervention should be minimized, it is essential for addressing certain abscesses, specific bowel obstructions, and cases of cancer. Regular colonoscopy screenings are advised every few years, starting eight years after the onset of the disease, to check for bowel cancer.
Crohn’s disease affects approximately 3.2 per 1,000 individuals in Europe, North America, and the UK. Its prevalence is lower in Asia and Africa. Historically, it has been more common in developed countries. However, rates have been steadily increasing since the 1970s, particularly in developing nations. Inflammatory bowel disease, including Crohn’s disease, accounted for 47,400 deaths in 2015. Individuals with Crohn’s disease typically have a slightly reduced life expectancy. While the disease commonly manifests during adolescence and early adulthood, it can occur at any age. Both males and females are equally affected by the condition.
Manifestations
Crohn’s disease can affect any segment of the gastrointestinal tract, encompassing both the small and large intestine. It may involve multiple segments or present as a continuous inflammation. In some cases, the disease solely affects the colon, which forms part of the large intestine.
The signs and symptoms of Crohn’s disease can vary in intensity from mild to severe. They typically emerge gradually, although in certain instances, they may suddenly appear without prior warning. There can also be periods of remission when no signs or symptoms are present.
During active phases of the disease, the following symptoms are commonly observed:
- Diarrhea
- Fever
- Fatigue
- Abdominal pain and cramping
- Presence of blood in the stool
- Formation of mouth sores
- Decreased appetite and weight loss
- Pain or discharge near the anus caused by inflammation leading to the development of a tunnel into the skin (fistula)
Additional signs and symptoms Individuals with severe Crohn’s disease may also experience symptoms beyond the confines of the intestinal tract, including:
- Inflammation of the skin, eyes, and joints
- Inflammation of the liver or bile ducts
- Formation of kidney stones
- Iron deficiency leading to anemia
Factors that Increase Risk
Several factors can contribute to an increased risk of developing Crohn’s disease. These may include:
Age: Although Crohn’s disease can occur at any age, it is more commonly diagnosed in individuals who are young. Most people are diagnosed with Crohn’s disease before the age of 30.
Ethnicity: While Crohn’s disease can affect individuals of any ethnic background, it is more prevalent among white populations, particularly those of Eastern European (Ashkenazi) Jewish descent. However, there has been an observed rise in the incidence of Crohn’s disease among Black populations in North America and the United Kingdom. Additionally, there is an increasing occurrence of the disease in the Middle Eastern population and among migrants to the United States.
Family history: Having a first-degree relative, such as a parent, sibling, or child, with Crohn’s disease increases your risk of developing the condition. Approximately 1 in 5 individuals with Crohn’s disease has a family member who also has the disease.
Cigarette smoking: Smoking is a significant modifiable risk factor for Crohn’s disease. It not only increases the likelihood of developing the condition but also leads to more severe disease and a higher risk of requiring surgical intervention. If you are a smoker, it is crucial to quit smoking.
Nonsteroidal anti-inflammatory medications: Certain medications like ibuprofen (Advil, Motrin IB, others), naproxen sodium (Aleve), diclofenac sodium, and others are classified as nonsteroidal anti-inflammatory drugs (NSAIDs). While these medications do not directly cause Crohn’s disease, they can exacerbate inflammation in the bowel, worsening the symptoms of Crohn’s disease.
It’s important to note that these risk factors may increase the likelihood of developing Crohn’s disease but do not guarantee its occurrence. It is a complex condition influenced by a combination of genetic, environmental, and immune factors.
References:
- Hovde Ø, Moum BA (April 2012). “Epidemiology and clinical course of Crohn’s disease: results from observational studies”. World Journal of Gastroenterology.
- Yamamoto-Furusho JK, Korzenik JR (November 2006). “Crohn’s disease: innate immunodeficiency?”. World Journal of Gastroenterology.
- Hanauer SB, Sandborn W (March 2001). “Management of Crohn’s disease in adults”. The American Journal of Gastroenterology.
- “What I need to know about Crohn’s Disease”. www.niddk.nih.gov.



























