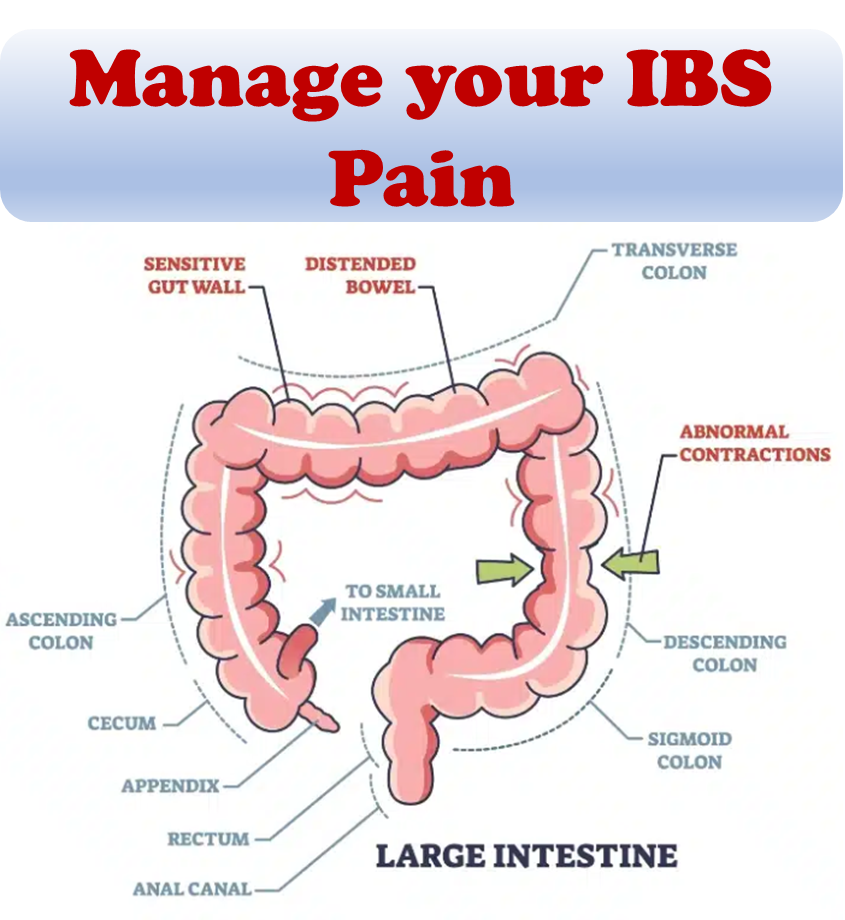
Dealing with irritable bowel syndrome (IBS) can be debilitating. Having to plan your daily routine around unpredictable bathroom habits can be challenging. While doctors often recommend a proper diet, sufficient sleep, and regular exercise to manage IBS symptoms, implementing these changes can be easier said than done for individuals struggling with the condition.
While medical intervention is crucial for treating IBS, making lifestyle and nutritional changes can also play a significant role in alleviating symptoms. In this article, we will explore nutritional changes that can help manage IBS symptoms. This will guide you through the steps to recovery and strategies for facing IBS challenges.
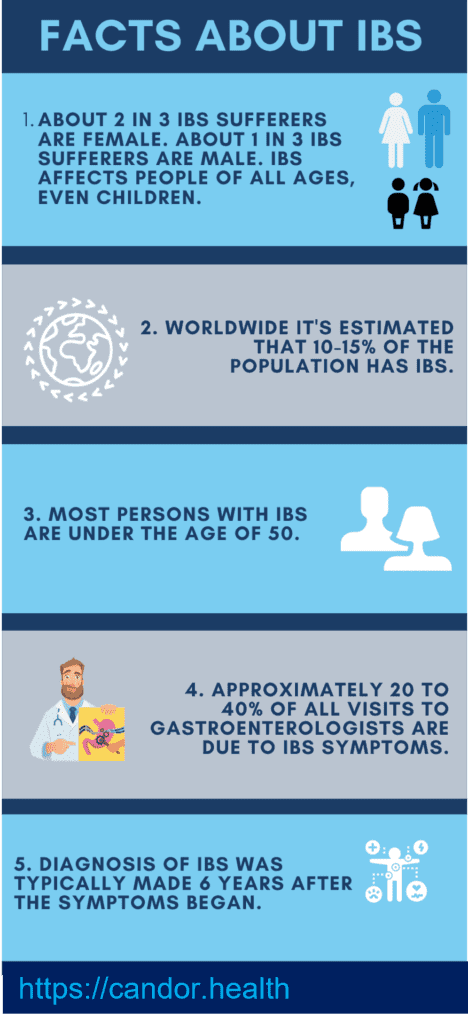
Prevalence
1. About 2 in 3 IBS sufferers are female. About 1 in 3 IBS sufferers are male. IBS affects people of all ages, even children.
2. Worldwide it’s estimated that 10-15% of the population has IBS.
3. Most persons with IBS are under the age of 50.
4. Approximately 20 to 40% of all visits to gastroenterologists are due to IBS symptoms.
5. Diagnosis of IBS was typically made 6.6 years after the symptoms began. (based on IFFGD survey)
Foods to limit:
Here’s a breakdown of the foods you should restrict:
- Lactose: Found in milk and dairy products like cream cheese, cottage cheese, ice cream, and sour cream. Consuming more lactose than your intestines can handle may result in abdominal pain and gas. Around half the global population has lower levels of lactase, the enzyme responsible for metabolizing lactose.
- Meat: Poultry and fish can be high in fat content and challenging to digest for individuals with IBS. Lean meats like chicken and turkey often contain growth hormones and toxins, which can disrupt hormonal balance. It is advisable to minimize meat consumption.
- Eggs: Eggs have a high sulfur content, which can promote the growth of inflammatory bacteria in the gut. They also trigger the release of TMAO (trimethylamine N-oxide), leading to symptoms of a leaky gut. Additionally, eggs are rich in cholesterol and may not be the most ideal source of protein.
- Vegetables: Certain vegetables can cause gas and abnormal bowel habits. High-FODMAP vegetables like garlic and onions should be temporarily avoided before gradually reintroducing them. It’s important not to completely eliminate these vegetables as they do offer health benefits.
- Oils: Oils are pure fats without fiber and essentially provide empty calories. They offer no significant benefits and can contribute to body fat accumulation and digestive discomfort. Consider exploring oil-free cooking methods whenever feasible.
- Polyols: Polyols are sugar substitutes commonly found in candy and sugarless gum. They can pose issues for individuals with severe IBS symptoms. Additionally, it’s important to avoid consuming jaggery, stevia, maple syrup, mannitol, sorbitol, maltitol, isomalt, and xylitol. Be vigilant about hidden sugars in packaged foods.
Foods to incorporate:
- Dairy-free alternatives: Opt for lactose-free milk options such as rice milk, oat milk, and soy milk. Similarly, consider dairy-free curds like coconut yogurt or peanut curd as alternatives.
- Low/Medium fructose fruits: Fruits offer antioxidants, phytosterols, and anti-inflammatory properties to support healing. Aim for 3-5 servings of fruits per day, including options like bananas, pineapples, cantaloupes, and berries.
- Low/Medium FODMAP vegetables: Include vegetables like green beans, carrots, eggplant, celery, yam, spinach, sweet potato, squash, and zucchini. Enhance their flavors with herbs such as chili, basil, ginger, coriander, mint, lemongrass, marjoram, oregano, rosemary, parsley, and thyme.
- Lentils/Pulses: Lentils are a fantastic food group that promotes the growth of beneficial gut bacteria. They stimulate the release of short-chain fatty acids (SCFAs), which contribute to gut healing and strengthening. If lentils are initially challenging to digest, soak them overnight, wash thoroughly, rinse with fresh water, and cook them well. Sprinkle some lemon juice before consumption to aid digestion. Aim for 2-3 servings of lentils per day.
- Ginger: Ginger exhibits anti-inflammatory and antioxidant effects that can alleviate IBS symptoms. Studies from PubMed Central suggest ginger’s potential benefits for digestive health, including reducing intestinal cramping, preventing indigestion, reducing bloating, and alleviating gas. Ginger is also known for its effectiveness in managing nausea, vomiting, diabetes, menstrual cramps, osteoarthritis, and migraines. However, more research is needed to fully understand its benefits for IBS symptoms. Recommended doses range from 500-2000 mg of ginger powder per day, usually taken during the first few days of the menstrual cycle. Mixing grated ginger with lemon and water and sipping on it 30 minutes after meals is a suggested approach.
- Peppermint oil: IBS can cause uncomfortable symptoms like gas, bloating, stomach cramps, pain, diarrhea, and constipation. Peppermint oil, a natural solution, may provide relief and improve digestion for IBS patients. However, the exact cause of IBS is unknown, and more research is necessary to determine the full potential of peppermint oil in treating IBS symptoms. There is no consensus on the best dose or form, but studies suggest daily doses of 1 to 2 grams of ginger powder per day. One approach is to grate a thumb-sized piece of ginger, extract the juice, mix it with lemon and water, and sip on it after meals.
- Cayenne pepper: Another effective treatment for IBS and chronic indigestion is the ingestion of cayenne pepper powder. Researchers evaluated the impact of orally administering red pepper on symptoms of visceral hypersensitivity in IBS patients. The study, conducted on 50 IBS patients, revealed that the group receiving red pepper scored better than the placebo group. Preliminary results suggested that chronic administration of enteric-coated red pepper powder in IBS patients was more effective than a placebo in decreasing the intensity of abdominal pain and bloating. Moreover, the patients themselves perceived cayenne pepper as more effective than a placebo.
- Complementary treatments for IBS encompass a range of approaches, including dietary changes, supplements, herbs, and behavior modifications.
IBS-related constipation – certain foods can exacerbate constipation associated with IBS. These include:
- White bread and cereals made from refined grains
- Processed foods like chips and cookies
- Alcohol, coffee, and carbonated drinks
- Diets high in animal protein
- Milk products, especially cheese
IBS-related diarrhea – certain foods can worsen IBS-related diarrhea. These include:
- Abruptly increasing fiber intake.
- Consumption of food and drinks containing alcohol, chocolate, caffeine, fructose, or sorbitol.
- Carbonated drinks.
- Large meals or infrequent eating patterns.
- Fried and fatty foods.
- Milk products.
- Wheat for individuals with Celiac’s disease.
Medications that can trigger IBS – in many cases, the medications clients are taking may contribute to their IBS symptoms. Here are some examples:
- Antibiotics.
- Certain antidepressants.
- NSAIDs.
- Medications containing sorbitol, such as cough syrup.
- Specific supplements, like iron, that can lead to constipation.
It is important to consult your doctor before making any changes to your medication regimen. They can help you switch to a medication that won’t exacerbate your symptoms. When it comes to antidepressants, be cautious in your selection. Tricyclic antidepressants, the older class of medications, may cause constipation, while selective serotonin reuptake inhibitors (such as fluoxetine and sertraline) can lead to diarrhea. Collaborating with your doctor will help identify the most suitable antidepressant for your needs.
Understanding the Role of Dairy in IBS
IBS is a complex condition with multiple potential triggers, including food allergies, food sensitivities, small intestinal bacterial overgrowth (SIBO), and gut dysbiosis. One common irritant to the gut is lactose, a sugar found in milk. As infants, we produce an enzyme called lactase that helps break down and digest lactose. However, many adults lose this enzyme after the age of two, making digesting dairy difficult and potentially triggering IBS symptoms. Some individuals may be more affected than others.
Interestingly, many people have reported the disappearance of their IBS symptoms within weeks of eliminating dairy from their diets. This suggests that lactose intolerance may be a more common issue than IBS itself.
Therefore, it is worth eliminating dairy from your diet for a few weeks and monitoring your progress. This includes avoiding milk, curds, ghee, butter, paneer, and cheese. To make the transition easier, familiarize yourself with dairy alternatives and start substituting dairy products with options like soy milk chai instead of dairy chai and peanut and rice milk curds instead of dairy curds. These alternatives are widely available for purchase globally or can be easily made at home.
Implementing a Low-FODMAP Diet
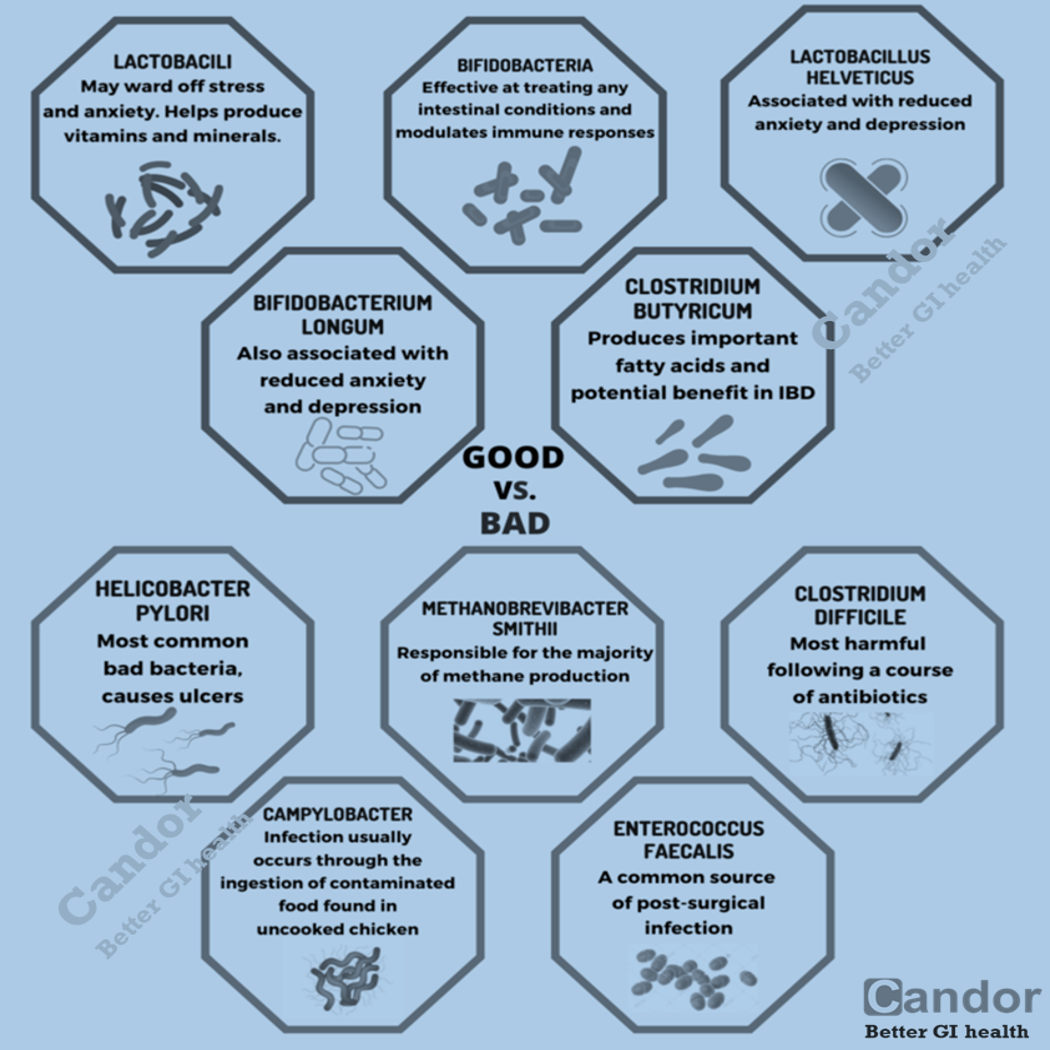
Once you have successfully transitioned to dairy-free alternatives, the next step is to focus on rebuilding a healthy population of beneficial bacteria in your gut. Many physicians recommend a low-FODMAP diet for individuals with IBS. FODMAP stands for “Fermentable Oligo Di Monosaccharides And Polyols.”
High-FODMAP foods are more difficult to digest, and when the undigested portions reach the intestines, they are metabolized by gut bacteria, leading to excessive gas production, diarrhea, abdominal pain, and constipation.
A low-FODMAP approach can provide temporary relief, akin to putting a bandage on a wound. While it may alleviate symptoms, it does not address the underlying issue of a weak gut function. To truly heal the gut, it is crucial to gradually reintroduce high-FODMAP foods, as this promotes gut bacterial diversity and fosters healing. It is important to remember that a low FODMAP diet is not meant to be a long-term solution. Prolonged adherence to a strict low FODMAP diet can further weaken the gut. Instead, focus on strategically reintroducing new foods to your diet on a weekly basis, gradually expanding your range of choices.
Keeping a food diary and documenting the types and quantities of food consumed, along with any adverse effects experienced, can be invaluable in identifying intolerances. Mobile apps like Candor can greatly help in this effort.
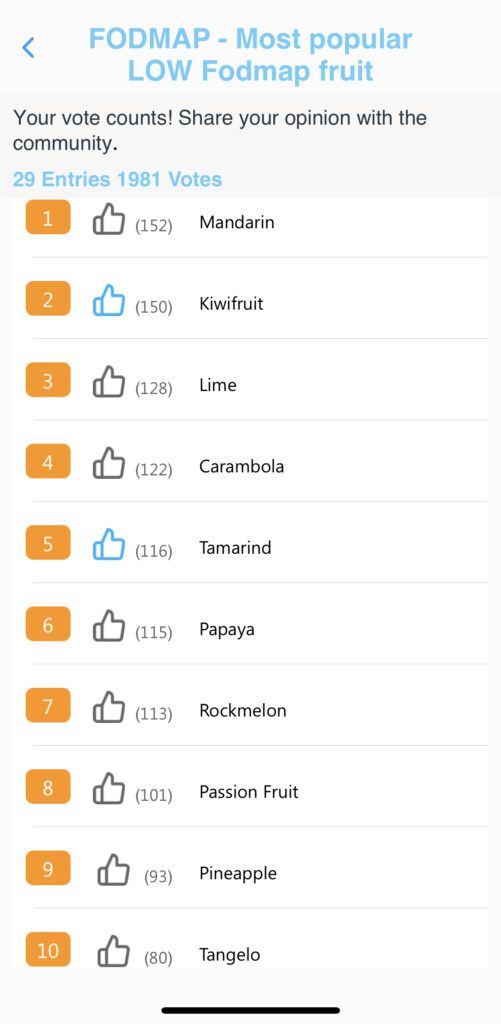
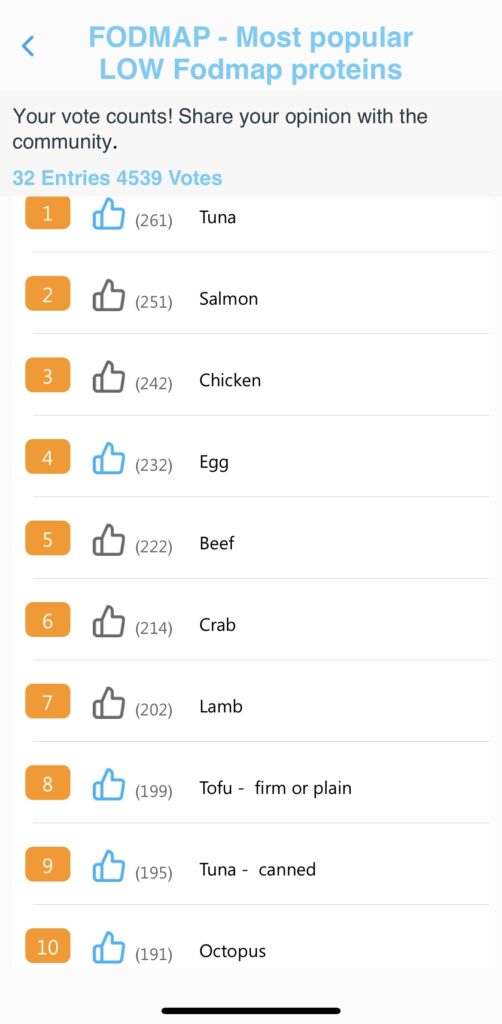
The Candor app allows you to stay on track with low FODMAP diet. Candor’s food and drink catalog includes labels to easily identify High/Medium/Low FODMAP foods. Candor app users can also understand the most logged low FODMAP foods (see below).

The role of fiber in IBS
Fiber can be beneficial for some individuals with IBS, but it can also exacerbate symptoms such as gas and diarrhea. However, it’s important to note that the symptoms are not caused by fiber itself, but rather by a poorly functioning gut. Interestingly, fiber is nourishment for the beneficial gut bacteria! It is best to slowly incorporate soluble fiber first, followed by insoluble fiber. It is ideal to start with a daily intake of 25 grams of fiber (~1 oz) and gradually increase it to around 60 grams (~2 oz).
Recent studies have shown that embracing fiber can support a healthy gut microbiome. Fiber supplementation has also been linked to increased levels of Bifidobacterium, which are crucial gut bacteria that aid in gut motility, immune function, insulin resistance, and maintaining a healthy weight.
For individuals with severe SIBO symptoms, mild prebiotic supplements can be beneficial in conjunction with antimicrobial protocols. For example, a clinical study involving people with SIBO found that combining the antibiotic rifaximin with guar gum eliminated SIBO in 87.1% of cases, compared to 62.1% when using antibiotics alone.
Most people seem to benefit from starting with Psyllium Husk or Benafiber supplementation while simultaneously encouraging lifestyle changes. It is also advisable to begin with predominantly soluble fiber sources before incorporating insoluble fiber. Soluble fiber dissolves in water, unlike insoluble fiber, which adds bulk to the stool. Good sources of soluble fiber include citrus fruits, barley, peas, and apples.
The effectiveness of a gluten-free diet
Gluten is a protein commonly found in grain products like wheat, rye, and barley. It can cause issues for individuals with gluten intolerance, such as those with Celiac’s disease. In such cases, adopting a gluten-free diet can help reduce symptoms. However, it’s important to note that wheat, just like other grains, actually possesses anti-inflammatory properties. According to Harvard Medical School, avoiding gluten without a diagnosed sensitivity can do more harm than good, as it further reduces the diversity of plant-based foods in your diet. Plant diversity is a crucial factor in maintaining gut health.
The impact of a low-fat Diet
Consistently consuming high-fat foods contributes to various health problems, including obesity. Fats are broken down in the body by an enzyme called lipase. In some cases of IBS, there may be low lipase production, resulting in an inability to properly digest fats, thereby exacerbating symptoms.
Another issue is that high-fat foods tend to be low in fiber. Embracing a low-fat diet not only benefits heart health but also improves uncomfortable bowel symptoms.
What about healthy fats? Aim to consume no more than 30-40 grams (~1-1.5 oz) of nuts/seeds spread throughout the day. Whenever possible, incorporate olives and avocados into your diet. These sources of healthy fats are sufficient for your needs. In my work with clients, I also assist them in exploring oil-free cooking techniques.
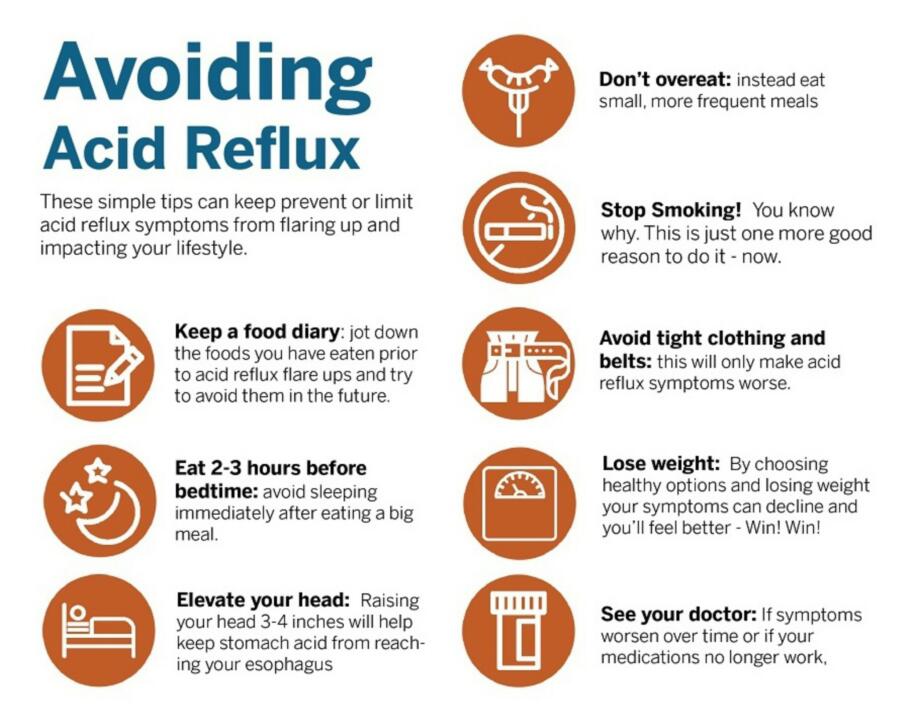
Stress and anxiety triggers for IBS
Stress and anxiety can exacerbate symptoms of IBS. This is because stress stimulates the release of cortisol from the adrenal glands, which has inflammatory properties and can contribute to increased inflammation. Some common stress factors include:
- Work-related stress
- Commuting challenges
- Home-related issues
- Financial difficulties
- A sense of loss of control
Managing stress
- Adopt healthy habits such as prioritizing sleep according to circadian rhythms (before 11 pm and waking up before 7 am) and engaging in regular exercise.
- Incorporate relaxation techniques or meditation into your routine.
- Learn effective stress management strategies through behavioral therapy. Consider therapies like relaxation therapy, hypnotherapy, biofeedback, psychotherapy, and cognitive-behavioral therapy.
Since everyone’s experience with IBS is unique, not all foods will be equally effective in managing symptoms. It’s important to assess your individual symptoms and consult your doctor before making any significant dietary changes. You may need to experiment with different foods and observe how your body responds to specific eating patterns. It is also recommended to stay hydrated, reduce caffeine intake, and engage in regular exercise to promote regularity and minimize IBS symptoms.
While medications can be used to treat IBS, a change in diet should be the first approach. Adopting a healthy lifestyle with a low-fat diet, regular exercise, and avoiding alcohol and smoking can make a significant difference. For those who still need further relief, diets like the low-FODMAP diet can be beneficial. Consider seeking guidance from a registered holistic nutritionist who can assist you in making optimal food choices. In some cases, your doctor may determine that medication is necessary to manage your IBS symptoms. These medications may include anticholinergic drugs or antidepressants to reduce stress and calm spasms.
Indian diet plan and lifestyle changes for managing IBS
Both diet and lifestyle changes play a crucial role in treating and controlling IBS. Before embarking on any changes, it’s important to understand your body. Keep a record of everything you eat and drink for 7 to 10 days, along with the timing, and note any symptoms you experience. Remember that food may not be the sole trigger. It is important to also explore some lifestyle changes that can be made alongside a sample meal plan.
- Fiber is a key nutrient for managing IBS, but it’s important to regulate your fiber intake based on your tolerance. Rapidly increasing fiber intake can lead to bloating and gas formation.
- Include a generous amount of seasonal vegetables and fruits in your diet. The recommendation is to aim for five servings per day for individuals with IBS symptoms. However, be cautious with fruit juices as they can worsen bloating and diarrhea, particularly when fructose is not absorbed and ferments in the colon.
- Consider incorporating prebiotics and probiotics into your routine. These can help promote the growth of “good” bacteria and support a healthy gut.
- Opt for plant-based protein sources such as pulses and soy. Well-cooked lentils like whole moong and masoor are preferable for individuals with mild loose motion.
- Reduce the consumption of foods high in both sugar and fats. Avoid the use of ghee, butter, and oil altogether.
- Stay adequately hydrated by drinking plenty of fluids. Aim for at least 2 liters of water per day and consider incorporating other hydrating options like herbal teas and coconut water.
- Limit your intake of caffeine and alcohol as excessive consumption of both can cause discomfort. Ideally, limit yourself to no more than two cups of tea or coffee per day, and avoid consuming them with or immediately after a meal.
- Avoid skipping meals and aim to eat at consistent times each day. Opt for smaller, frequent meals throughout the day, and incorporate 2-3 snacks. Research has shown that larger meals can worsen IBS symptoms. Remember to chew your food thoroughly, eat slowly, and take time to relax after each meal.
- Try to have your dinner early. Engage in regular exercise and activities such as walking, cycling, or swimming.
- Incorporate relaxation techniques into your routine. This can include practices such as meditation or mindfulness.
By implementing these Indian diet plan and lifestyle changes, you can effectively manage your IBS symptoms and improve your overall well-being. However, it’s always recommended to consult with a healthcare professional or registered dietitian for personalized guidance and support.
Summary
Adopting a plant-centric, low FODMAP diet may require some effort and learning. It involves eliminating certain foods while incorporating others. Seeking guidance from healthcare professionals or nutritionists can ease the transition to the FODMAP diet. The time and effort invested in making these changes are worthwhile. Moreover, dietary modifications such as veganism or a low FODMAP diet offer healthy alternatives. Consulting a professional can assist in designing a well-balanced diet that meets your nutritional needs.
References:
- Gibson PR, Shepherd SJ (February 2010). “Evidence-based dietary management of functional gastrointestinal symptoms: The FODMAP approach”. Journal of Gastroenterology and Hepatology.
- Barrett JS (March 2017). “How to institute the low-FODMAP diet”. Journal of Gastroenterology and Hepatology (Review).
- Gibson PR (March 2017). “History of the low FODMAP diet”. Journal of Gastroenterology and Hepatology (Review).
- Biesiekierski JR, Rosella O, Rose R, Liels K, Barrett JS, Shepherd SJ, Gibson PR, Muir JG (April 2011). “Quantification of fructans, galacto-oligosacharides and other short-chain carbohydrates in processed grains and cereals”. Journal of Human Nutrition and Dietetics.