Managing Crohn’s disease involves following a carefully tailored Crohn’s diet and working with a qualified Crohn’s dietician. Crohn’s disease causes inflammation in the digestive tract, affecting the gastrointestinal (GI) tract from the mouth to the anus. This inflammation leads to symptoms like watery diarrhea, abdominal cramping, fever, nausea, vomiting, and intestinal bleeding. Weight loss can occur due to poor appetite, increased nutritional needs, or difficulties in nutrient absorption. Scar tissue in the GI tract, known as strictures, can further hinder nutrient consumption.
During flare-ups of Crohn’s disease, it is recommended to follow a low residue/low fiber Crohn’s diet to alleviate digestive stress.
Although specific foods do not directly cause flare-ups, certain foods may exacerbate symptoms for some individuals. To provide the bowel with a chance to rest during these times, it is advised to limit fiber intake.
Conversely, during symptom-free periods, transitioning to a high-fiber Crohn’s diet is beneficial. A high-fiber diet promotes normal gastrointestinal function and strengthens the intestinal walls. Including a variety of fruits, vegetables, and whole grains in your diet on a regular basis when you are not experiencing a flare-up supports overall good health.
While Crohn’s disease does not have direct dietary causes, it is important to address individual food intolerances. Working with a knowledgeable Crohn’s dietician can help personalize your diet based on specific food intolerances that may contribute to your symptoms.
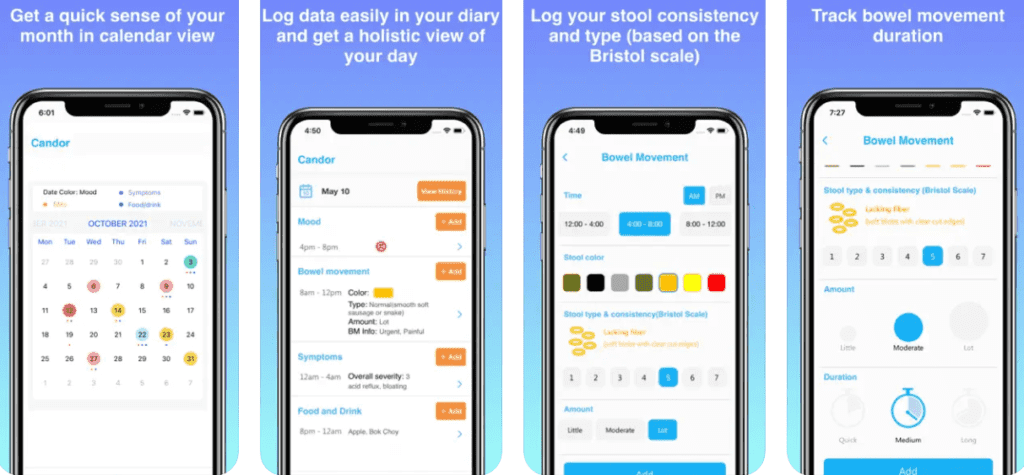
Keeping a food diary and documenting the types and quantities of food consumed, along with any adverse effects experienced, can be invaluable in identifying these intolerances. Mobile apps like Candor (see screens below) can greatly help in this effort.
Here are some revised guidelines for your Crohn’s diet:
- Opt for small, frequent meals every 3 to 4 hours, and be sure not to skip any meals.
- Stay hydrated by drinking at least 8-10 cups of fluids daily to compensate for fluid loss due to diarrhea.
- If you experience steatorrhea (fatty loose stools), it may be helpful to limit your fat intake. Consult your Crohn’s dietician about incorporating a Medium Chain Triglyceride (MCT) supplement.
- If you are lactose intolerant, consider reducing your consumption of milk and milk products or trying lactose-free alternatives. To ensure adequate calcium intake, discuss calcium with vitamin D supplements with your healthcare team.
- Avoiding seeds, nuts, corn hulls, and raw fruits and vegetables is advisable if you have strictures.
- Including foods with probiotics (such as kefir and yogurt) and prebiotics (like bananas) in your Crohn’s diet could be beneficial.
- It is best to avoid spicy foods.
- Collaborating with a Crohn’s dietician is crucial in determining the potential benefits of incorporating supplemental vitamins and minerals into your regimen. During episodes of inflammation, patients may find value in including multivitamins, folate, B6, and B12 supplements.
- Engage in a conversation with your doctor or Crohn’s dietician to explore the possibility of introducing a probiotic supplement, which can contribute to supporting the health of beneficial gut bacteria.
- If you are currently taking methotrexate or sulfasalazine, it is advised to supplement your daily intake with an additional 1mg of folic acid, except on the day methotrexate is administered.
- To optimize your dietary choices during periods of inflammation remission, it is advisable to incorporate an appropriate amount of fiber. Aim for a daily intake of 25-35 grams of fiber. Your Crohn’s dietician can provide you with a comprehensive list of high fiber foods that can assist you in achieving your dietary goals.
- Strive for a well-balanced Crohn’s diet that includes foods rich in antioxidants, such as blueberries, artichokes, and pecans. Additionally, consider incorporating Omega-3 fatty acids from sources like salmon, flax seeds, and walnuts.
- When gradually increasing fiber intake, it is beneficial to do so over time to minimize the occurrence of gas and bloating. Remember to increase your fluid intake alongside the fiber increase.
- To ensure a smooth transition, introduce only 1 to 2 new foods to your Crohn’s diet per week. Begin with small amounts and carefully monitor your symptoms. If any adverse symptoms arise, discontinue consuming the new food. You can re-evaluate and attempt it again after a few weeks.
Remember, working with a qualified Crohn’s dietician is essential in developing a personalized Crohn’s diet plan that meets your specific needs and supports your overall well-being.
References:
- Baumgart DC, Sandborn WJ (August 2012). “Crohn’s disease”. Lancet.
- “Crohn’s Disease”. National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK).
- Lichtenstein GR, Loftus EV, Isaacs KL, Regueiro MD, Gerson LB, Sands BE (April 2018). “ACG Clinical Guideline: Management of Crohn’s Disease in Adults”. The American Journal of Gastroenterology.
- Molodecky NA, Soon IS, Rabi DM, Ghali WA, Ferris M, Chernoff G, Benchimol EI, Panaccione R, Ghosh S, Barkema HW, Kaplan GG (January 2012). “Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review”. Gastroenterology.



























