
Irritable bowel syndrome (IBS) causes digestive, abdominal discomfort and/or changes in the pattern of bowel movements without any evidence of underlying damage. IBS sufferers will have a group of symptoms, but tests won’t show any physical explanation for those problems. IBS has evolved into a very common gastrointestinal disorder that affects 1 in 7 people. The causes are not well understood, and it is diagnosed based on ruling out other conditions with similar symptoms. Diet and lifestyle modifications are the best option at present, and some medications may help as well. IBS is a chronic condition that can be controlled, but not cured. For an in-depth overview of IBS, check out our overview on IBS.
Essential guidelines for following an Indian diet for IBS
- Embrace probiotics: Make it a daily habit to incorporate probiotics into your diet to promote a healthy gut.
- Steer clear of common food triggers: Avoid high FODMAP foods that can aggravate IBS symptoms and stay away from fatty foods, alcohol, carbonated beverages, caffeine, and chocolate.
- Implement a low FODMAP diet: Begin with the elimination phase to remove high FODMAP foods from your meals. Proceed to the reintroduction phase to identify specific triggers. Personalize your diet based on your individual tolerance levels during the personalization phase.
- Opt for smaller, frequent meals: Instead of large meals, consume six smaller meals throughout the day to support digestion.
- Practice mindful eating: Slow down and chew your food thoroughly, avoiding distractions such as television or mobile devices during meals.
- Say no to artificial sweeteners and smoking: Eliminate artificial sweeteners from your diet and quit smoking to support overall health and IBS management.
- Engage in regular exercise: Dedicate 45 minutes to 1 hour each day to exercise. Choose activities that you enjoy, such as walking, swimming, cycling, yoga, or any sport that interests you.
- Reduce stress levels: Incorporate stress-reducing practices like meditation, listening to music, or reading a book. Connect with loved ones and engage in a five-minute conversation with your best friend to significantly reduce stress.
- Prioritize quality sleep: Ensure you get adequate and restful sleep to support your overall well-being and manage IBS symptoms effectively.
- Embrace local, seasonal, and organic produce: Include a variety of fresh, locally sourced, seasonal fruits and vegetables in your diet. Opt for organic options to minimize exposure to potentially harmful substances.
These guidelines can help you effectively navigate an Indian Low FODMAP IBS diet and support your digestive health and overall well-being.
Can the Indian diet for IBS help ease symptoms?
While consulting a physician and undergoing medical tests to determine specific trigger foods is recommended, there are several commonly used diets to alleviate uncomfortable IBS symptoms.
- Elimination Diet: The International Foundation for Functional Gastrointestinal Disorders (IFFGD) recommends the elimination diet as a starting point for newly diagnosed IBS patients. This diet focuses on removing four common trigger foods from the diet: coffee, chocolate, insoluble fiber, and nuts. By eliminating one food at a time for a period of 12 weeks and observing any improvements in symptoms, individuals can identify specific trigger foods and exclude them from their diet.
- Low FODMAP Diet: The low FODMAP diet is widely recognized and effective in managing IBS symptoms. FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) are carbohydrates that can draw excess water into the bowel, leading to gas, bloating, and diarrhea. The low FODMAP diet involves limiting high FODMAP foods to reduce symptoms.
- Low-Fat Diet: A low-fat diet is beneficial for individuals with mixed IBS symptoms, which combine constipation and diarrhea. High-fat foods can exacerbate symptoms and contribute to various health issues, including obesity. Embracing a low-fat diet aids in weight loss, promotes heart health, and improves uncomfortable bowel symptoms. Avoid red meat, deep-fried foods, junk foods, and full-fat dairy products. Instead, include lean meats, fruits, vegetables, grains, and low-fat dairy options.
- Gluten-Free Diet: Gluten, a protein found in certain grains, can cause issues for individuals intolerant or sensitive to it. In such cases, gluten should be completely avoided. A gluten-free diet entails excluding wheat, barley, rye, and foods containing these grains. Instead, opt for gluten-free alternatives like rice, millets, buckwheat, flax seeds, quinoa, and tapioca (sabudana).
- Fiber Diet: Fiber plays a crucial role in bulking up stool and promoting proper bowel movements. The recommended daily fiber intake for adults is around 20-35 grams. Soluble fiber is particularly helpful in treating IBS symptoms, while insoluble fiber can cause discomfort. Therefore, it is important to consume insoluble fiber in moderation. Adequate water intake is essential when consuming fiber-rich foods. Insoluble fiber sources include whole grains, nuts, tomatoes, raisins, cabbage, and broccoli, while soluble fiber sources include parboiled rice, leafy vegetables, berries, apples, and oats.
While these diets have shown promise in reducing IBS symptoms for many individuals, it is important to remember that what works for one person may not work for another. Consulting with a healthcare professional and seeking personalized advice is crucial when creating an IBS diet plan tailored to your specific needs.
In-depth look at Low FODMAP diet
The FODMAP concept was first published in 2005 as part of a hypothesis paper. In this paper, it was proposed that a collective reduction in the dietary intake of all indigestible or slowly absorbed, short-chain carbohydrates would minimize stretching of the intestinal wall. This was proposed to reduce stimulation of the gut’s nervous system and provide the best chance of reducing symptom generation in people with IBS. At the time, there was no collective term for indigestible or slowly absorbed, short-chain carbohydrates, so the term ‘FODMAP’ was created to improve understanding and facilitate communication of the concept.
For a full overview of the origin of the low FODMAP diet, check this article.
What are the benefits of low FODMAP diet? Can it be adapted to an Indian diet for IBS?
The low-FODMAP diet has proven to be beneficial for thousands of people worldwide, as supported by several studies that have demonstrated its positive impact on overall quality of life. Many patients following this diet have also reported increased energy levels. FODMAP is an acronym that stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols. These are short-chain carbohydrates that resist digestion and instead remain in the intestine, where the majority of gut bacteria reside. Gut bacteria utilize these carbohydrates as fuel, resulting in the production of gas, which can lead to symptoms such as bloating and other discomforts in individuals with IBS. In some cases, FODMAPs can also draw liquid from the intestine, causing diarrhea.
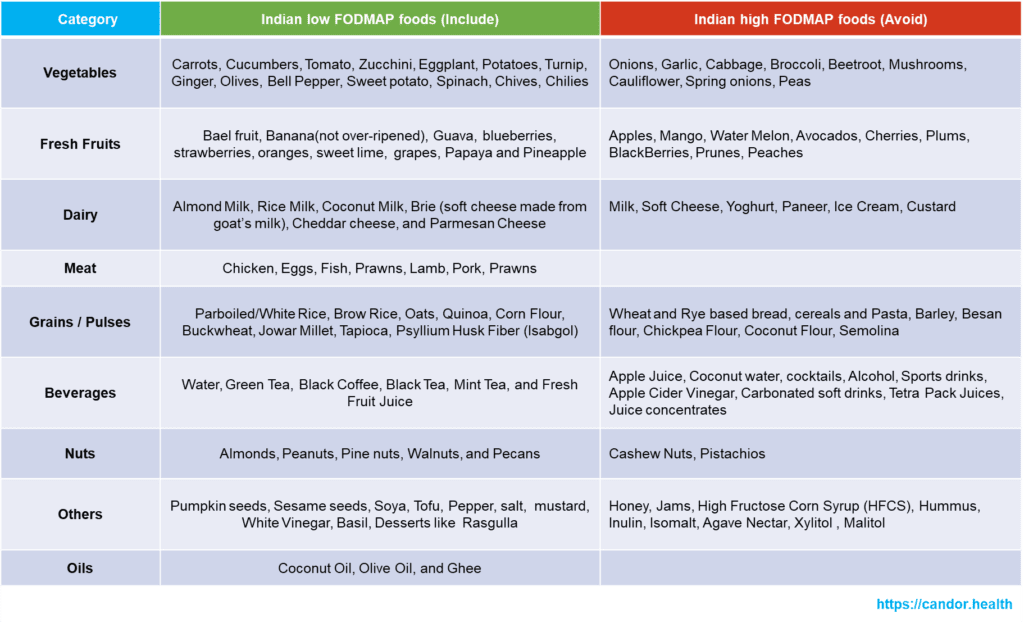
Therefore, the low-FODMAP diet involves excluding foods that are high in FODMAPs. Common examples of FODMAPs include fructose, which is a simple sugar found in many fruits, vegetables, and various sugar forms; lactose, present in dairy products like milk; fructans, found in foods such as wheat, rye, spelt, and barley; galactans, which are found in large amounts in legumes; and polyols, which are sugar alcohols such as xylitol, sorbitol, maltitol, mannitol, and sorbitol. It is important to note that not all carbohydrates fall into the high-FODMAP category, so there’s no need to eliminate all foods in this category. The low-FODMAP diet should be followed for a duration of 8-12 weeks to achieve proper results.
To effectively plan a low-FODMAP diet and avoid overly restrictive meals, it is highly recommended to consult with a qualified nutritionist or dietitian. They can provide guidance and support in creating the best diet plan for managing IBS.
How can I adapt the Indian diet for IBS to be low FODMAP?
A low FODMAP diet consists of three stages that aim to effectively manage symptoms:
Stage 1: Restriction
During this initial stage, all high FODMAP foods are strictly eliminated from the diet. This phase typically lasts for 3-8 weeks, although some individuals may experience relief as early as the first week, while others may require the full 8 weeks to notice any changes. If there is no improvement in symptoms after this period, it is advisable to consult a gastroenterologist. While high FODMAP foods must be completely eliminated, low FODMAP foods can be consumed judiciously.
Stage 2: Reintroduction
The purpose of this stage is to systematically reintroduce high FODMAP foods back into the diet.
The main objectives of this stage are:
- Identifying FODMAP types that are well-tolerated by the individual.
- Establishing the threshold value for each particular FODMAP food, which indicates the amount that can be consumed without triggering symptoms.
During this stage, specific foods are tested one at a time over the course of three consecutive days. Foods that are well-tolerated are gradually reintroduced. It is important to continue following a restricted diet during this stage, and seeking guidance from a qualified dietitian or nutritionist is highly recommended.
Stage 3: Personalization
This stage involves creating a personalized diet plan based on the individual’s tolerance levels for various FODMAPs identified in the second stage.
Once an individual reaches this stage, they can add more variety to their diet. This increased variety and flexibility can lead to improvements in gut health and overall quality of life. By progressing through these stages and receiving guidance from healthcare professionals, individuals can effectively manage their symptoms and enjoy a well-balanced and personalized diet. Here is a summarized view of the options in an Indian diet for IBS:
What are the risks and limitations of the Indian diet for IBS adapted to be low FODMAP?
The low FODMAP diet is a specialized approach for individuals diagnosed with Irritable Bowel Syndrome (IBS) to identify and manage foods that trigger their symptoms. While it has proven to be effective in IBS management, it is important to understand the limitations associated with this diet. For a look at the risks, check our article on the topic.
– A low-FODMAP diet is highly restrictive in various groups of nutrients, can be impractical to follow in the long-term and may add an unnecessary financial burden. The low FODMAP diet can be highly restrictive, as it involves the elimination of various types of carbohydrates. This restriction may impact the enjoyment and variety of meals, potentially leading to challenges in adhering to the diet long term. It is essential to seek guidance from a healthcare professional or dietitian to ensure a balanced and diverse diet within the limitations of the low FODMAP approach.
– A low-FODMAP diet might help to improve short-term digestive symptoms in adults with irritable bowel syndrome, but its long-term use can have negative effects because it causes a detrimental impact on the gut microbiota and metabolome. It should only be adopted for short periods of time and under the advice of a specialist.
- The use of a low-FODMAP diet without medical advice can lead to serious health risks, including nutritional deficiencies and misdiagnosis, so it is advisable to conduct a complete medical evaluation before starting a low-FODMAP diet to ensure a correct diagnosis and that the appropriate therapy may be undertaken.
– Since the consumption of gluten is suppressed or reduced with a low-FODMAP diet, the improvement of the digestive symptoms with this diet may not be related to the withdrawal of the FODMAPs, but of gluten, indicating the presence of an unrecognized celiac disease, avoiding its diagnosis and correct treatment.
– Not a long-term or sustainable diet. The low FODMAP diet is not intended to be followed in the long term. It is designed as an elimination and reintroduction protocol to identify specific trigger foods. Once trigger foods are identified, the goal is to reintroduce a variety of foods to achieve a balanced diet. It is important to work with a qualified healthcare professional or dietitian to transition to a sustainable long-term eating plan.
– The low FODMAP diet can inadvertently reduce the intake of prebiotics, which are beneficial for gut health. Prebiotics are non-digestible fibers that nourish the beneficial bacteria in the gut. While the diet aims to alleviate IBS symptoms, it is important to incorporate alternative sources of prebiotics or consider probiotic supplements to support a healthy gut microbiome.
– Potential for nutritional deficiencies. Individuals with additional food allergies or dietary restrictions may face challenges in meeting their nutritional needs while following the low FODMAP diet. The elimination of certain food groups can increase the risk of nutrient deficiencies if not carefully managed. It is crucial to work with a qualified healthcare professional or dietitian to ensure adequate nutrient intake and address any potential deficiencies through appropriate supplementation or alternative food choices.
While the low FODMAP diet has proven to be effective in managing symptoms of IBS, it is important to be aware of its limitations. Consulting with a healthcare professional or registered dietitian is essential to navigate these limitations and develop a personalized approach that ensures optimal nutrition and overall well-being.
References:
- Gibson PR, Shepherd SJ (February 2010). “Evidence-based dietary management of functional gastrointestinal symptoms: The FODMAP approach”. Journal of Gastroenterology and Hepatology.
- Barrett JS (March 2017). “How to institute the low-FODMAP diet”. Journal of Gastroenterology and Hepatology (Review).
- Gibson PR (March 2017). “History of the low FODMAP diet”. Journal of Gastroenterology and Hepatology (Review).
- Biesiekierski JR, Rosella O, Rose R, Liels K, Barrett JS, Shepherd SJ, Gibson PR, Muir JG (April 2011). “Quantification of fructans, galacto-oligosacharides and other short-chain carbohydrates in processed grains and cereals”. Journal of Human Nutrition and Dietetics.



























